
Medication & Alcohol Interaction Checker
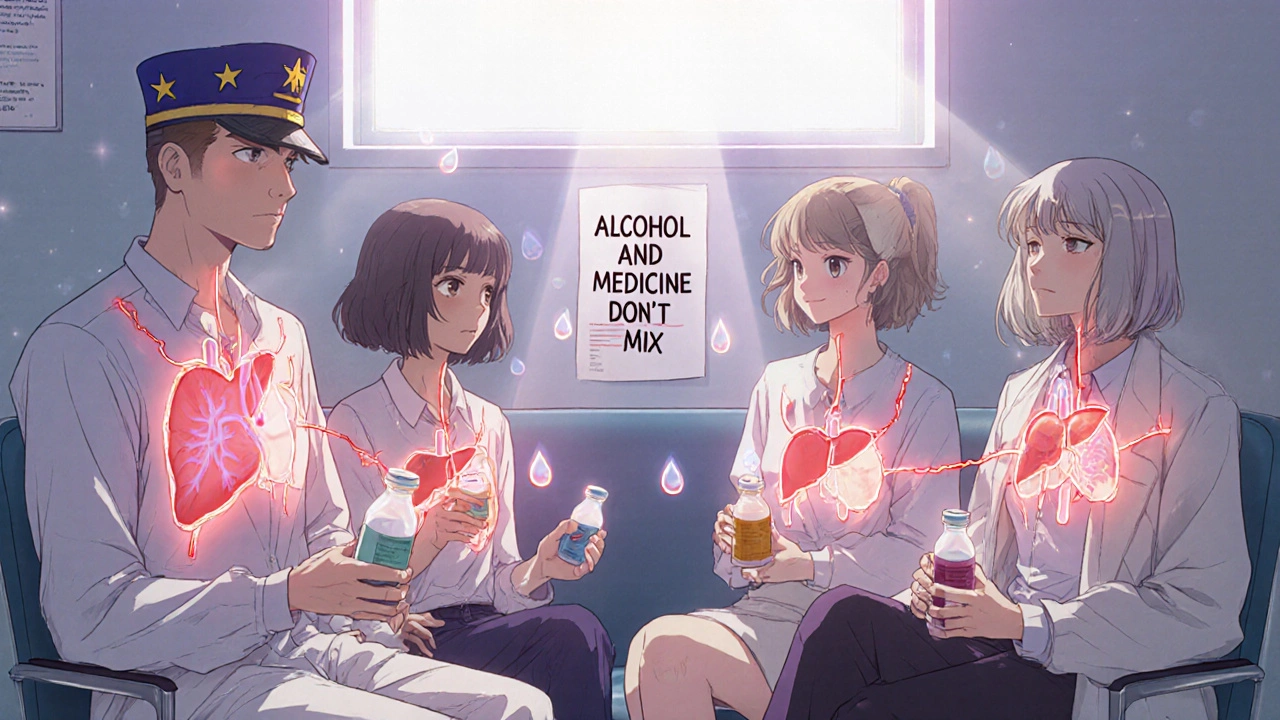
Every year, thousands of people end up in emergency rooms-not from accidents or infections, but from something many assume is harmless: mixing alcohol with their medications. It’s not just about getting drunk faster. It’s about your liver shutting down, your breathing slowing to a stop, or your blood pressure dropping so low you pass out and can’t get up. And the scariest part? Most people don’t realize they’re putting themselves at risk.
How Alcohol Changes How Your Medications Work
Alcohol doesn’t just sit there while your pills do their job. It actively interferes. The liver is the main battlefield. About 90% of alcohol is broken down there by enzymes like CYP2E1 and ADH. But so are dozens of common medications-painkillers, antidepressants, antibiotics, blood pressure drugs. When alcohol is in your system, it competes for the same enzymes. This can mean two things: your medication builds up to dangerous levels, or it gets flushed out too fast and stops working.Take acetaminophen, the active ingredient in Tylenol. On its own, it’s safe when taken as directed. But with alcohol, the liver starts producing a toxic byproduct called NAPQI. Normally, your body neutralizes it with glutathione. But alcohol depletes glutathione fast. Without it, NAPQI starts destroying liver cells. The FDA says this combo causes about 56,000 emergency room visits and nearly 500 deaths each year in the U.S. alone. You don’t need to be a heavy drinker. Even one drink while taking a standard dose of acetaminophen can push you into danger.
The Deadliest Mixes: Opioids, Benzodiazepines, and Alcohol
Some combinations don’t just make you dizzy-they can kill you in minutes. Opioids like oxycodone, hydrocodone, and methadone already slow your breathing. So does alcohol. Together, they amplify each other. The FDA pulled the extended-release opioid Palladone off the market in 2005 after studies showed alcohol caused a sudden, massive release of the drug-dosing patients with up to six times the intended amount. In 2020, 20% of opioid overdose deaths also involved alcohol, according to the CDC.Benzodiazepines like Xanax, Valium, and Ativan work the same way. They calm your nervous system. Add alcohol, and you’re not just feeling relaxed-you’re risking respiratory arrest. A 2019 study in the Journal of Substance Abuse Treatment found that mixing these drugs with alcohol increases overdose risk by 24 times. This isn’t theoretical. Emergency rooms see it every weekend: someone takes a pill for anxiety, has a drink at dinner, and doesn’t wake up.
Other High-Risk Medications You Might Not Suspect
You might think only strong prescription drugs are dangerous. But many common OTC and even herbal products carry serious risks.- NSAIDs (ibuprofen, naproxen): These are fine alone. But with alcohol, they increase your risk of stomach bleeding by 3 to 5 times. The lining of your stomach gets worn down faster, and your blood can’t clot properly. This isn’t just an upset stomach-it can mean internal bleeding that requires surgery.
- Metronidazole (Flagyl): This antibiotic causes a violent reaction with alcohol: flushing, vomiting, rapid heartbeat, chest pain. It’s called a disulfiram-like reaction. You’ll feel awful within minutes. The Illinois Poison Center says wait at least 72 hours after your last dose before drinking.
- Antihistamines (Benadryl, Zyrtec): They already make you drowsy. Alcohol makes it worse. You could fall asleep while driving, trip and break a bone, or stop breathing during sleep. GoodRx reports that 60% of people using these meds don’t know alcohol makes drowsiness worse.
- ADHD meds (Adderall, Ritalin): These are stimulants. Alcohol is a depressant. Mixing them tricks your brain into thinking you’re not as drunk as you are. You might drink more, raise your heart rate dangerously, and increase your risk of heart attack or stroke.
- Diabetes drugs (sulfonylureas, metformin): Alcohol can cause your blood sugar to crash-sometimes to life-threatening levels. Sulfonylureas like glipizide increase hypoglycemia risk by 300% when mixed with alcohol. Metformin can trigger lactic acidosis, a rare but deadly buildup of acid in the blood.
Why Older Adults Are at Highest Risk
If you’re 65 or older, your body handles alcohol and drugs differently. Your liver and kidneys don’t work as fast. Your body has less water, so alcohol concentrates more in your blood. You’re also more likely to be on multiple medications. The CDC says adults over 65 fill an average of 14 prescriptions a year. Eighty-two percent of them take at least one drug that interacts dangerously with alcohol.The Beers Criteria, updated in 2019 by the American Geriatrics Society, lists 30 medications that are especially risky for seniors-like benzodiazepines, muscle relaxants, and first-gen antihistamines. These can cause falls, confusion, and hospitalization. A 2022 study in JAMA Internal Medicine found that only 35% of primary care doctors routinely ask older patients about alcohol use. That means most seniors aren’t warned.
Women and Veterans: Hidden Vulnerabilities
Women metabolize alcohol slower than men. Even if you weigh the same, you’ll have higher blood alcohol levels after the same drink. That means medication interactions hit harder and faster. The NIAAA says women are more likely to suffer liver damage from alcohol-medication combos.Veterans face another layer of risk. The VA’s 2021 report found that 30% of veteran suicides involved alcohol and prescription drugs. Many are on opioids for chronic pain, benzodiazepines for PTSD, and antidepressants-all of which can interact dangerously. The same goes for people with mental health conditions. SAMHSA reports that those with co-occurring disorders are 3.5 times more likely to experience harmful interactions.
What You Can Do to Stay Safe
You don’t have to give up alcohol entirely-but you do need to know the rules.- Read every label. The FDA requires warning labels on about 100 prescription drugs and 700 over-the-counter products. Look for phrases like "avoid alcohol," "may cause drowsiness," or "do not consume with alcohol."
- Ask your pharmacist. They’re the most accessible experts. A 2023 survey found 70% of pharmacists see patients daily who don’t know their meds interact with alcohol.
- Wait 72 hours after antibiotics. Especially metronidazole, tinidazole, or certain cephalosporins. Don’t guess-wait.
- Use the AUDIT-C screen. It’s a simple three-question tool doctors use to spot risky drinking. Ask your provider to use it during your next visit.
- Keep a medication list. Include all prescriptions, OTC drugs, vitamins, and herbal supplements. Bring it to every appointment.
Some people think, "I only have one glass of wine." But one drink can be enough to trigger a reaction with certain meds. The CDC’s "Alcohol and Medicine Don’t Mix" campaign, launched in January 2023, aims to change this mindset. It’s not about being perfect-it’s about being informed.
New Tools Are Helping Prevent Tragedies
Technology is catching up. Electronic health records like Epic now have hard-stop alerts. If a doctor tries to prescribe an opioid to someone who drinks, the system flashes a warning. Insurance companies are starting to require alcohol use screening before filling high-risk prescriptions.Even more promising: genetic testing. Researchers found that people with a specific variant of the CYP2E1 enzyme are 4.7 times more likely to suffer liver damage from acetaminophen and alcohol. While this isn’t routine yet, it’s coming. In the future, your DNA might tell you whether you’re at higher risk before you even take a pill.
Bottom Line: When in Doubt, Skip the Drink
There’s no safe amount of alcohol with many medications. Even if you’ve mixed them before without issue, your body changes. Your liver ages. Your meds change. Your tolerance shifts. What was fine last year could be deadly this year.If you’re taking any medication-prescription, over-the-counter, or herbal-assume alcohol is unsafe until proven otherwise. Talk to your doctor. Ask your pharmacist. Read the label. And if you’re unsure? Don’t risk it. One drink isn’t worth a hospital stay, a liver transplant, or your life.
Can I have one drink while taking Tylenol?
It’s not safe. Even one drink can increase your risk of liver damage when taking acetaminophen. The liver can’t process both at the same time, leading to toxic buildup. The FDA warns that acetaminophen-alcohol combinations cause hundreds of deaths each year. Avoid alcohol completely while using Tylenol or any product containing acetaminophen.
How long should I wait after taking metronidazole before drinking alcohol?
Wait at least 72 hours after your last dose. Metronidazole causes a severe reaction with alcohol-nausea, vomiting, rapid heartbeat, and flushing. This reaction can happen even if you drink a small amount hours after taking the drug. The Illinois Poison Center and FDA both recommend the 72-hour window to be safe.
Does alcohol make antidepressants less effective?
Yes. Alcohol is a depressant and can worsen symptoms of depression and anxiety. It can also reduce the effectiveness of SSRIs like sertraline or fluoxetine. Some people feel worse emotionally after drinking while on antidepressants, and the risk of suicidal thoughts increases. Even moderate drinking can interfere with treatment.
Are herbal supplements safe with alcohol?
Not always. St. John’s Wort can interact with alcohol and increase drowsiness. Kava, used for anxiety, has been linked to liver damage-and alcohol makes that risk much worse. Valerian root can amplify sedative effects. Many herbal products aren’t tested for alcohol interactions, so assume they’re risky unless proven otherwise.
Why do older adults face higher risks?
As we age, our liver and kidneys process alcohol and drugs more slowly. We also have less body water, so alcohol becomes more concentrated. Older adults often take multiple medications, increasing the chance of dangerous combinations. The Beers Criteria lists 30 drugs that are especially risky for seniors, including benzodiazepines and antihistamines, which can cause falls, confusion, and even death when mixed with alcohol.
Can I drink alcohol while on blood pressure medication?
It depends, but it’s risky. Alcohol can cause your blood pressure to drop suddenly, especially when combined with meds like beta-blockers or ACE inhibitors. This can lead to dizziness, fainting, and falls-especially dangerous for older adults. Some people experience severe orthostatic hypotension, where blood pressure crashes when standing up. Limit alcohol to one drink per day at most, and only if your doctor says it’s okay.






There are 13 Comments
Bailey Sheppard
This post is a wake-up call. I never realized how many everyday meds interact with alcohol. I used to have a glass of wine with my Tylenol, thinking it was fine. Now I’m switching to ibuprofen when I can, and even then I’m careful. Knowledge is power, and this is the kind of info that saves lives.
Kristi Joy
I’m a nurse and I see this every week. People come in confused, saying they only had one drink. One drink is enough. The worst part? They’re often elderly and on five different meds. No one ever tells them. Please, if you’re on anything, ask your pharmacist. They’re not just filling prescriptions-they’re keeping you alive.
Louie Amour
Let’s be real-this is just another government scare tactic wrapped in medical jargon. People have been drinking with meds for decades. If you’re dumb enough to mix metronidazole and whiskey, you deserve what you get. Stop infantilizing adults with fearmongering. My grandfather drank wine with his blood pressure meds until he was 92. He was fine.
Kristina Williams
Did you know the FDA is working with Big Pharma to make you afraid of alcohol so you’ll buy more meds? Alcohol is natural. Pills are chemicals. The liver can handle both if you’re not a weakling. They don’t want you to know that the real danger is the profit motive behind all these warnings. I stopped taking my antidepressants and now I just drink. I feel better.
Shilpi Tiwari
From a pharmacokinetic standpoint, the CYP450 enzyme competition is well-documented, particularly CYP2E1 and CYP3A4 isoforms. The competitive inhibition leads to altered clearance kinetics, resulting in elevated plasma concentrations of co-administered agents. Additionally, ethanol induces oxidative stress via ROS generation, depleting glutathione reserves-this is particularly critical in acetaminophen hepatotoxicity. The disulfiram-like reaction with nitroimidazoles involves aldehyde dehydrogenase inhibition, leading to acetaldehyde accumulation. These are not anecdotal-they’re mechanistically validated.
Denny Sucipto
I used to think drinking was just part of being an adult. Then my buddy passed out after mixing his Xanax with a beer. He woke up in the hospital. That changed everything. Now I don’t touch anything with alcohol. I tell everyone I know. It’s not about being perfect-it’s about being smart. One drink isn’t worth losing your life over. Seriously, just say no.
Holly Powell
It’s amusing how this post conflates correlation with causation. The CDC data cited is observational-confounding variables like polypharmacy, socioeconomic status, and comorbid mental illness are never controlled for. The 24x overdose risk? That’s from a small cohort study with selection bias. And don’t get me started on the ‘one drink is enough’ rhetoric-it’s emotional manipulation disguised as public health. Real science demands nuance, not fear.
Emanuel Jalba
THIS IS WHY AMERICA IS DYING 😭 People are dying because they don’t listen! My cousin died last year from mixing painkillers and wine. He was 28. I cry every time I think about it. PLEASE STOP. I don’t care if you’re 80 or 20-alcohol + meds = death. I’m begging you. Just say no. 🙏💔
Sarah Frey
Thank you for this meticulously researched and clinically grounded exposition. The inclusion of evidence-based guidelines, such as the Beers Criteria and the AUDIT-C screening tool, elevates this beyond anecdotal commentary. It is imperative that healthcare providers integrate alcohol-use assessments into routine care, particularly for geriatric populations. This is not merely a behavioral issue-it is a systemic gap in patient education.
Katelyn Sykes
Just got back from my grandpa’s place he’s 78 and on 7 meds he asked me if red wine is okay with his heart pills I told him no way and he laughed said he’s been doing it for 30 years I showed him this post he’s now reading the labels and even called his doctor wow what a difference one post makes
Gabe Solack
Big shoutout to pharmacists. I went in last week to pick up my metronidazole and asked about alcohol. The pharmacist pulled up my full med list, flagged three other interactions I didn’t know about, and even printed me a little cheat sheet. That’s the kind of care we need more of. Don’t just trust your doctor-talk to the person who actually knows the drugs inside out.
Yash Nair
why do americans make everything so scary its just one drink you people are so weak i drink with all my meds in india no one dies we have real problems here like poverty and corruption not this nonsense
Bailey Sheppard
Reading your comment made me realize something. I used to think the same way until I saw what happened to my cousin. It’s not about being weak-it’s about being alive. One drink might be fine for you. But for someone else? It’s a death sentence. We’re not all the same. That’s why the warning exists.
Write a comment
Your email address will not be published. Required fields are marked *