
Dapsone vs. Alternatives Comparison Tool
Primary Use: Leprosy, Dermatitis Herpetiformis
Typical Dose: 100 mg daily
Side Effects:
- Hemolytic Anemia
- Methemoglobinemia
- DRESS Syndrome
Special Considerations: Avoid in G6PD deficiency
Primary Use: Acne, Rosacea, Infections
Typical Dose: 50-100 mg BID
Side Effects:
- Photosensitivity
- Vestibular Issues
Special Considerations: Safe for G6PD deficiency
Primary Use: Multidrug-resistant Leprosy
Typical Dose: 100 mg daily
Side Effects:
- Skin Discoloration
- GI Upset
Special Considerations: Often paired with Rifampicin & Dapsone
Primary Use: Leprosy, TB, Prophylaxis
Typical Dose: 600 mg daily
Side Effects:
- Liver Toxicity
- Orange Body Fluids
Special Considerations: Induces drug interactions
Primary Use: Ulcerative Colitis, Rheumatoid Arthritis
Typical Dose: 500-1000 mg BID
Side Effects:
- GI Upset
- Rash
- Oligospermia
Special Considerations: May worsen sulfa allergy
Primary Use: Gout Flares, Familial Mediterranean Fever
Typical Dose: 0.6 mg BID
Side Effects:
- Diarrhea
- Neutropenia
Special Considerations: Renal dose adjustment needed
Recommendations Based on Your Selection
Select a condition above to get personalized recommendations comparing Dapsone with alternatives.
When your doctor prescribes Dapsone is a sulfonamide antibiotic used for leprosy, dermatitis herpetiformis, and certain skin infections, you might wonder if there’s a safer or more effective option. Whether you’re managing chronic skin disease, battling a stubborn infection, or minimizing side‑effects, knowing the trade‑offs between Dapsone and its rivals can save you months of trial‑and‑error.
Quick Takeaways
- Dapsone works well for leprosy and dermatitis herpetiformis but can cause hemolysis, especially in G6PD‑deficient patients.
- Minocycline and tetracycline are good first‑line oral options for acne‑type skin conditions and have a lower risk of blood disorders.
- Clofazimine and rifampicin are the standard combo for multi‑drug‑resistant leprosy, offering faster bacterial clearance.
- Sulfasalazine and colchicine serve niche roles (inflammatory bowel disease, gout) and may be useful when Dapsone is contraindicated.
- Choosing the right drug hinges on the disease being treated, patient genetics, and tolerance for side‑effects.
What Is Dapsone?
Dapsone belongs to the sulfone antibiotics class. It blocks bacterial synthesis of dihydrofolic acid, a key step for mycobacteria and certain gram‑positive organisms. Besides leprosy, the drug shines in treating dermatitis herpetiformis, a blistering rash linked to gluten sensitivity. Typical oral dosing starts at 100mg daily, but the regimen can be tweaked based on disease severity and patient weight.
Why Look at Alternatives?
While Dapsone is effective, it carries a handful of red flags. Hemolytic anemia, methemoglobinemia, and a rare hypersensitivity syndrome (DRESS) are serious concerns. Moreover, patients with glucose‑6‑phosphate dehydrogenase (G6PD) deficiency are at heightened risk of red‑cell breakdown. If you’ve experienced these issues or simply want a drug with a gentler side‑effect profile, it makes sense to compare the options.
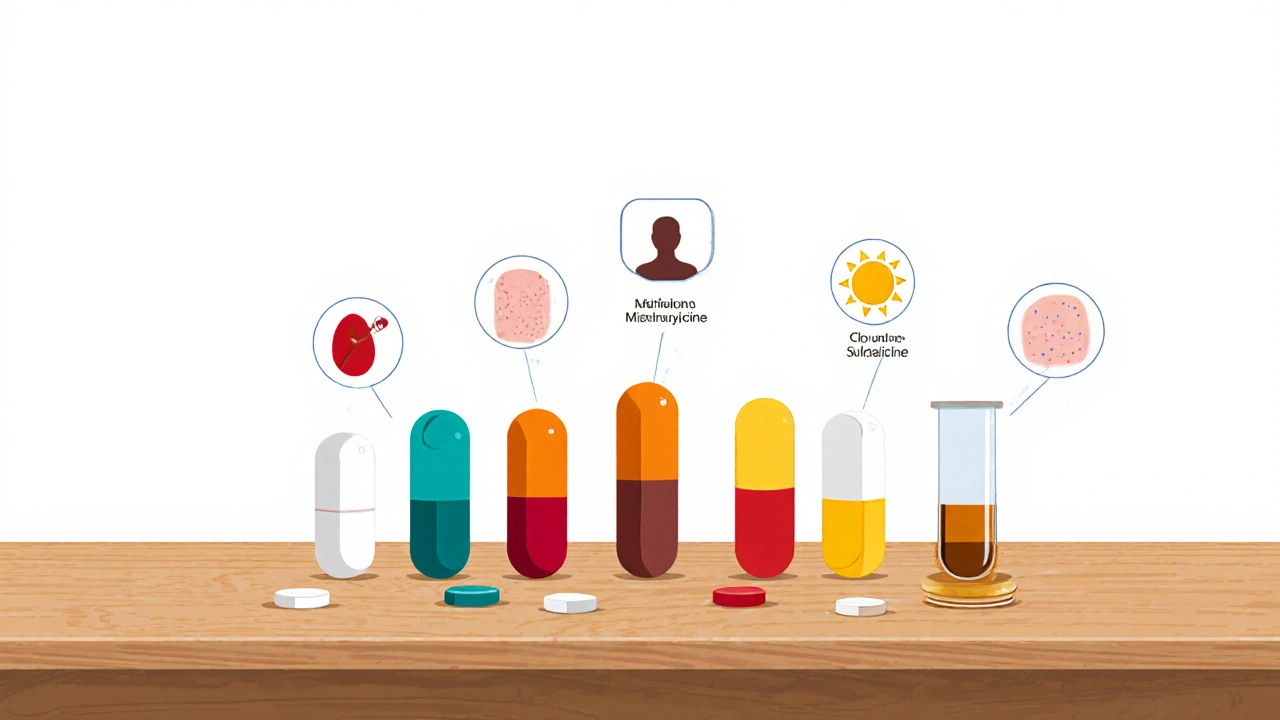
Top Alternatives at a Glance
| Drug | Primary Use | Typical Dose | Major Side‑effects | Special Considerations |
|---|---|---|---|---|
| Minocycline | Acne, rosacea, some infections | 50‑100mg BID | Photosensitivity, vestibular issues | Safe for G6PD deficiency |
| Clofazimine | Multidrug‑resistant leprosy | 100mg daily | Skin discoloration, GI upset | Often paired with rifampicin & Dapsone |
| Rifampicin | Leprosy, TB, bacterial prophylaxis | 600mg daily (leprosy) | Liver toxicity, orange body fluids | Induces many drug interactions |
| Sulfasalazine | Ulcerative colitis, rheumatoid arthritis | 500‑1000mg BID | GI upset, rash, oligospermia | May worsen sulfa allergy |
| Colchicine | Gout flares, familial Mediterranean fever | 0.6mg BID | Diarrhea, neutropenia | Renal dose adjustment needed |
| Tetracycline | Acne, rosacea, Lyme disease | 250‑500mg QID | Photosensitivity, esophagitis | Avoid in pregnancy, children <8y |
Deep Dive Into Each Alternative
Minocycline
Minocycline is a tetracycline‑class antibiotic with strong anti‑inflammatory properties. It’s often the go‑to for moderate‑to‑severe acne because it reduces both bacterial load and inflammatory lesions. Compared with Dapsone, minocycline doesn’t provoke hemolysis and works well for patients who can’t tolerate sulfa drugs. However, long‑term use may lead to vestibular side‑effects (dizziness, tinnitus) and a rare lupus‑like syndrome.
Clofazimine
Clofazimine is a phenazine dye with bactericidal activity against Mycobacterium leprae. In the World Health Organization’s 2024 leprosy treatment guidelines, it’s paired with Dapsone and rifampicin for multibacillary disease. The upside is a potent kill‑rate for resistant strains; the downside is marked skin hyperpigmentation that can be socially distressing.
Rifampicin
Rifampicin blocks bacterial RNA polymerase. It’s a cornerstone of both leprosy and tuberculosis regimens. When combined with Dapsone, it shortens treatment duration dramatically. Side‑effects include liver enzyme spikes and vivid orange discoloration of bodily fluids, which can alarm patients if they’re not warned ahead.
Sulfasalazine
Sulfasalazine blends a sulfonamide with a 5‑aminosalicylic acid. Though not a direct skin‑disease drug, it’s an alternative for patients who need anti‑inflammatory action but can’t use Dapsone due to blood‑disorder risk. Its main drawbacks are GI upset and potential infertility in men (oligospermia), so regular monitoring is advised.
Colchicine
Colchicine disrupts microtubule formation, curbing neutrophil migration. It’s most famous for gout, but dermatologists sometimes employ it for neutrophilic dermatoses that mimic Dapsone‑responsive rashes. Renal impairment mandates dose cuts; otherwise, diarrhea and bone‑marrow suppression are the chief concerns.
Tetracycline
Tetracycline is the older sibling of minocycline. It’s cheaper and works well for mild‑to‑moderate acne and certain tick‑borne infections. Photosensitivity is a big issue-patients need diligent sunscreen use. Pregnant women and young children should avoid it due to tooth discoloration risk.
How to Choose the Right Option
Start by asking three practical questions:
- What condition am I treating? Leprosy needs a multi‑drug combo (Dapsone+Clofazimine+Rifampicin). Acne or dermatitis herpetiformis often respond to minocycline or tetracycline.
- Do I have any genetic or health constraints? G6PD deficiency or liver disease push you toward minocycline or sulfasalazine.
- How much side‑effect risk can I tolerate? If cosmetic changes (orange fluids, skin darkening) are a deal‑breaker, skip rifampicin or clofazimine.
Talk with your prescriber about blood‑work frequency. For Dapsone, baseline hemoglobin, liver enzymes, and G6PD testing are essential. Alternatives usually require liver function monitoring (rifampicin) or renal checks (colchicine).
Common Pitfalls & How to Avoid Them
- Skipping baseline labs. A missed G6PD screen can lead to severe hemolysis.
- Combining drugs that share metabolic pathways. Rifampicin induces CYP3A4 and can lower levels of oral contraceptives, statins, and some antivirals.
- Ignoring photoprotection. Minocycline, tetracycline, and even Dapsone increase sun sensitivity; daily SPF30+ is a must.
- Expecting instant relief. Most dermatologic conditions need 4‑8weeks of consistent dosing before noticeable improvement.
Next Steps for Patients and Clinicians
If you’re currently on Dapsone and experiencing side‑effects, schedule a blood test and discuss an alternative strategy with your dermatologist or infectious‑disease specialist. For new patients, the decision tree below can guide the initial prescription:
- Diagnose disease (leprosy, dermatitis herpetiformis, acne, etc.).
- Screen for G6PD deficiency, liver and kidney function.
- Select first‑line drug based on efficacy and safety profile.
- Set monitoring schedule (CBC, LFTs, renal panel).
- Re‑evaluate at 4‑6weeks; switch if adverse events arise.
Frequently Asked Questions
Can I take Dapsone and minocycline together?
Generally no. Combining two sulfonamide‑related antibiotics increases the risk of blood disorders and doesn’t provide additive benefit for most skin conditions. If a clinician wants to use both, it’s usually for a short‑term overlap while switching.
What is the safest alternative for a patient with G6PD deficiency?
Minocycline or tetracycline are the preferred oral choices because they do not trigger hemolysis. For leprosy, the WHO recommends adding clofazimine and rifampicin while omitting Dapsone.
How long does it take to see improvement with Dapsone for dermatitis herpetiformis?
Most patients report a significant reduction in itching and blister formation within 2‑4weeks of a consistent 100mg daily dose, provided they also follow a strict gluten‑free diet.
Does clofazimine cause permanent skin darkening?
The pigmentation can be long‑lasting and sometimes permanent, especially after prolonged therapy. Patients should be counseled before starting, and some clinicians reserve clofazimine for cases where other drugs have failed.
Are there any OTC options that work like Dapsone?
No over‑the‑counter product matches Dapsone’s antibacterial strength for leprosy or dermatitis herpetiformis. For mild acne, topical benzoyl peroxide or salicylic acid can be useful, but they don’t treat the underlying immune component.






There are 16 Comments
Lily Tung
Dapsone has historically occupied a central role in the treatment of leprosy and dermatitis herpetiformis. Its mechanism of action involves inhibition of dihydrofolic acid synthesis thereby compromising bacterial replication. Nevertheless the drug’s adverse effect profile necessitates careful patient selection particularly in the context of G6PD deficiency. Hemolytic anemia represents a frequent hematologic complication that can culminate in clinical instability. Methemoglobinemia further complicates the therapeutic landscape by impairing oxygen delivery. The rare yet severe DRESS syndrome imposes additional monitoring requirements during prolonged therapy. In contrast minocycline offers a comparable antimicrobial spectrum with a distinctly disparate side effect constellation. Phototoxicity and vestibular disturbances rank among the most commonly reported adverse events associated with minocycline. Importantly minocycline does not precipitate hemolysis and thus circumvents the principal hematologic hazard of dapsone. Clofazimine, while effective against multidrug‑resistant Mycobacterium leprae, is burdened by cutaneous discoloration and gastrointestinal upset. The drug’s propensity to accumulate in fatty tissues underlies its prolonged half‑life and delayed clearance. Rifampicin complements both dapsone and clofazimine by expediting bacterial eradication but introduces hepatic toxicity and potent enzyme induction. Sulfasalazine and colchicine occupy niche positions in the therapeutic armamentarium serving inflammatory bowel disease and gout respectively. Their side effect profiles are dominated by gastrointestinal irritation and neutropenia which must be weighed against clinical benefit. Ultimately the selection of an appropriate agent demands individualized assessment of disease manifestation, genetic predispositions and tolerance for adverse effects.
Taryn Bader
The drama of picking a skin drug feels like a soap opera!
Myra Aguirre
I see the chart and it’s clear that each medicine has its own trade‑off. Dapsone works well for leprosy but the blood issues can scare people. Minocycline seems safer for acne lovers who want fewer lab worries. The table helps a lot when you’re trying to compare side effects.
Shawn Towner
One might assume that the newest alternatives automatically trump dapsone, yet the evidence does not always support such a sweeping claim. The literature shows that in certain leprosy regimens dapsone remains indispensable. It is convenient to dismiss older drugs as obsolete without acknowledging their unique pharmacodynamics. Moreover the side‑effect profile, while noteworthy, is manageable under proper monitoring. Thus the narrative of dapsone being merely a relic is oversimplified.
Ujjwal prakash
Whoa, look at that comparison table-so many options, so much info, and yet it’s kinda overwhelming! Dapsone, minocycline, clofazimine, rifampicin-all those names pop up, each with its own quirks. If you’re G6PD‑deficient, definitely steer clear of dapsone, but don’t forget minocycline can cause photosensitivity-watch out in summer! Bottom line: read the side‑effects, talk to your doc, and pick what fits your lifestyle.
Diane Helene Lalande
I appreciate the thorough breakdown; it really clarifies when each drug shines. For patients wary of blood‑related side effects, highlighting minocycline as a safer alternative is helpful. Thanks for the clear presentation.
Edwin Levita
While you pontificate on the “indispensable” nature of dapsone, you overlook the lived experience of those battling severe anemia. The drama is not in the literature but in the patient’s bedside.
Xander Laframboise
From a pharmacological perspective, dapsone’s sulfone structure confers both anti‑mycobacterial activity and oxidative stress potential. This duality explains why it excels in leprosy yet predisposes to hemolysis in G6PD‑deficient individuals. Minocycline’s tetracycline core, on the other hand, lacks this oxidative burden, making it a preferable choice for acne where safety is paramount. Clofazimine’s lipophilicity accounts for its characteristic skin discoloration as the drug deposits in subcutaneous fat. Therefore, understanding the chemical underpinnings informs rational drug selection beyond superficial efficacy.
Jason Petersen
Sounds good but you ignore real‑world adherence issues and cost barriers.
Melissa Gerard
Honestly this whole table looks like a marketing brochure 🙄.
Cindy Knox
The way the side‑effects are listed feels like a roller‑coaster ride of emotions-one minute you’re hopeful about dapsone, the next you’re terrified of anemia! It’s a wild ride.
beverly judge
It helps to separate the emotional reaction from the clinical data; the table provides a factual baseline you can rely on when the roller‑coaster descends.
Capt Jack Sparrow
Look, the key takeaway is that no single drug covers all bases; you need a regimen tailored to the disease, genetics, and side‑effect tolerance.
Manju priya
Dear readers, I encourage you to consult your healthcare provider and review these options carefully; an informed decision empowers better outcomes 😊.
Jesse Groenendaal
Just stating the obvious doesn’t add value.
Persephone McNair
From a pharmacokinetic standpoint, the bioavailability variance among dapsone, minocycline and clofazimine necessitates dose optimization algorithms to mitigate adverse event incidence while maximizing therapeutic index.
Write a comment
Your email address will not be published. Required fields are marked *