
Triptan-SSRI Safety Checker
For patients with migraine who also take antidepressants, this tool helps determine if combining triptans with SSRIs or SNRIs is safe based on current medical evidence.
Result will appear here
After clicking 'Check Safety'
For over 15 years, patients with migraine who also take antidepressants have been told they can’t use triptans. The reason? A warning from the FDA in 2006 about serotonin syndrome - a rare but serious condition caused by too much serotonin in the brain. But here’s the truth: triptans and SSRIs are almost certainly safe to take together. The fear isn’t backed by real-world evidence. It’s based on theory, not data.
What’s the real risk?
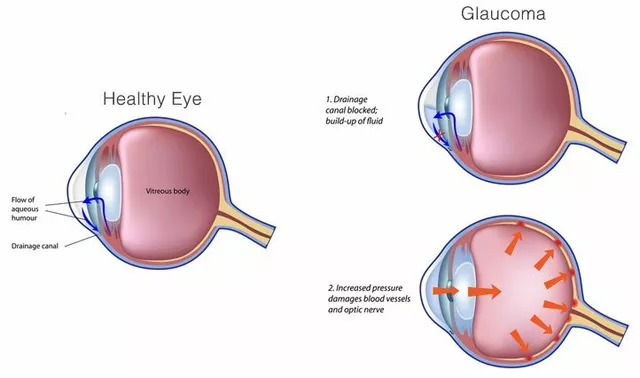
Serotonin syndrome happens when your nervous system gets flooded with serotonin. Symptoms can include shivering, high fever, fast heart rate, muscle stiffness, confusion, and in severe cases, seizures or death. It’s dangerous - but it’s also extremely rare. Most cases happen when someone takes two drugs that strongly boost serotonin at the same time, like an MAOI with an SSRI, or an overdose of a single drug. Triptans, like sumatriptan or rizatriptan, are designed to treat migraines. They work by targeting specific serotonin receptors - 5-HT1B and 5-HT1D - to shrink swollen blood vessels around the brain. They don’t increase serotonin levels in the brain. They just activate certain receptors already there. SSRIs, like sertraline or fluoxetine, do something different. They block the reabsorption of serotonin, so more of it stays in the spaces between nerve cells. That’s how they help with depression and anxiety. But even with SSRIs alone, serotonin syndrome is uncommon. Studies show it occurs in about 0.5 to 0.9 cases per 1,000 patient-months with some SSRIs. The problem? Triptans don’t cause serotonin overload. They don’t stimulate the receptors that trigger serotonin syndrome - especially 5-HT2A, the main villain in this condition. So even if you’re on an SSRI, adding a triptan doesn’t push you over the edge. It’s like turning on a single light in a room with a dimmer switch - not flipping every switch at once.The FDA warning: a mistake based on theory
In 2006, the FDA issued a safety alert saying combining triptans and SSRIs could lead to serotonin syndrome. That warning changed everything. Pharmacists started refusing to fill prescriptions. Doctors stopped prescribing triptans to patients on antidepressants. Patients were left without effective migraine relief. But here’s the kicker: the FDA didn’t have any real cases to back it up. They based their warning on lab studies and theoretical pharmacology - not actual patient data. And over the next 17 years, science caught up. A landmark 2019 study in JAMA Neurology looked at 61,029 patients who took both triptans and SSRIs or SNRIs over nearly three decades. Zero cases of serotonin syndrome met the strict diagnostic criteria. Not one. Not even a close call. Dr. P. Ken Gillman, a leading expert on migraine and serotonin, wrote in 2010: “There is neither significant clinical evidence, nor theoretical reason, to entertain speculation about serious serotonin syndrome from triptans and SSRIs.” He called the FDA’s warning a misunderstanding with “wide ramifications.”What do real doctors do?
If you ask a neurologist who treats migraines every day, they’ll tell you the same thing: we prescribe triptans with SSRIs all the time. No special monitoring. No extra warnings. Just a standard prescription. A 2021 survey of 250 headache specialists found that 89% routinely prescribe triptans to patients on SSRIs or SNRIs. That’s not because they’re reckless. It’s because they’ve seen the data. They’ve treated thousands of patients. They’ve watched for symptoms. And they’ve found nothing. The American Headache Society updated its guidelines in 2022: “Clinicians should not avoid prescribing triptans to patients taking SSRIs or SNRIs due to theoretical concerns.” That’s not a suggestion. It’s a clear directive based on evidence. Even UpToDate, the go-to clinical reference used by doctors worldwide, now says the risk is “negligible.” The European Medicines Agency never issued the same warning - because they looked at the same data and decided it didn’t hold up.
Why does the myth still exist?
Because technology doesn’t always keep up with science. Many pharmacy computer systems still flag triptan-SSRI combinations as “high risk.” Pharmacists get alerts. They call the doctor. They refuse to fill the script. Patients get confused. They think, “If the system says it’s dangerous, it must be true.” A 2022 survey by the American Migraine Foundation found that 42% of migraine patients on SSRIs had been denied a triptan prescription - not because they had symptoms, but because their pharmacist or doctor was afraid. Not one of those patients had ever experienced serotonin syndrome. Reddit threads, Facebook groups, and patient forums are full of stories: “My pharmacist wouldn’t fill my sumatriptan because I’m on Zoloft.” “My neurologist said no, even though I’ve been on both for years.” “I’ve had migraines for 15 years and never felt anything weird - but now I’m scared to take my medicine.” The Migraine Foundation of New Zealand even ran a quiz in 2024 asking: “Is serotonin toxicity likely when a SSRI is co-prescribed with a triptan?” The correct answer? False. And they’re still fighting misinformation.What’s changing now?
The tide is turning. In 2023, the American Headache Society and the National Headache Foundation formally petitioned the FDA to remove the warning. They cited 17 years of data showing no real risk. The FDA’s own adverse event database from 2006 to 2022 recorded only 18 possible cases - and after expert review, none were confirmed as true serotonin syndrome. Meanwhile, the number of people taking triptans with SSRIs has actually gone up. In 2007, only 18.7% of triptan prescriptions were filled for patients also on SSRIs. By 2022, that number jumped to 32.4%. More doctors are prescribing. More patients are getting relief. And still, no surge in serotonin syndrome cases. Even drug manufacturers are adjusting. The 2023 prescribing information for Imitrex (sumatriptan) still mentions the FDA warning - but now adds: “Epidemiological studies have not shown an increased risk of serotonin syndrome with concomitant use of triptans and SSRIs/SNRIs.” The Mayo Clinic, once cautious, now says: “The theoretical risk has not materialized in clinical practice.”
What should you do if you’re on both?
If you take an SSRI or SNRI for depression or anxiety and get migraines, here’s what you need to know:- You can safely take triptans. The risk of serotonin syndrome is not meaningfully higher than if you were taking an SSRI alone.
- Don’t let a pharmacist or outdated system deny you treatment. Ask your doctor to write a note explaining the evidence.
- If you’ve been on both for months or years without issues, you’re fine. Don’t stop your migraine meds out of fear.
- Know the signs of serotonin syndrome - but understand they’re extremely unlikely here. Symptoms include sudden fever, muscle rigidity, rapid heartbeat, confusion, or seizures. If you experience these, seek help - but don’t assume it’s from your meds.
The bigger cost of this myth
This isn’t just about one drug interaction. It’s about how fear can hurt patients. When people can’t use triptans, they turn to less effective options: NSAIDs, opioids, or expensive new migraine drugs like CGRP inhibitors. Some go untreated. Some end up in the ER. Some lose work days. A 2020 study estimated this single misunderstanding cost the U.S. healthcare system $450 million a year in unnecessary treatments and lost productivity. It’s not just money. It’s quality of life. Migraine is one of the most disabling conditions in the world. For someone with depression and migraines, triptans are often the only thing that gives them back control. Denying them based on a myth isn’t safety - it’s neglect.Final takeaway
The science is clear. Triptans and SSRIs together are safe. The FDA warning was based on guesswork. The data that followed proved it wrong. Doctors know it. Patients are learning it. The system is slowly catching up. If you’re on an SSRI and have migraines, talk to your doctor. Ask: “Is there any real reason I can’t take a triptan?” If they say yes, ask them to show you the evidence. Chances are, they won’t be able to. You don’t have to choose between treating your mood and treating your pain. You can do both - safely.Can you get serotonin syndrome from taking triptans and SSRIs together?
No - not in any meaningful way. While the FDA issued a warning in 2006, large studies of tens of thousands of patients have found zero confirmed cases of serotonin syndrome from this combination. Triptans activate specific serotonin receptors (5-HT1B/1D) used for migraine relief, but they don’t trigger the 5-HT2A receptors responsible for serotonin syndrome. SSRIs increase serotonin levels, but even alone, serotonin syndrome is rare. Together, the risk remains negligible.
Why do pharmacists still refuse to fill triptans if I’m on an SSRI?
Because many pharmacy computer systems still use outdated alerts based on the 2006 FDA warning. These systems haven’t been updated to reflect the latest evidence. Pharmacists are trained to respond to alerts, so they often call the doctor or refuse the prescription out of caution - even though current guidelines from the American Headache Society and UpToDate say it’s safe. You may need to ask your doctor to write a note explaining the evidence.
What are the real symptoms of serotonin syndrome?
Serotonin syndrome involves three key areas: mental changes (confusion, agitation, hallucinations), autonomic hyperactivity (high blood pressure, fast heart rate, sweating, fever), and neuromuscular issues (tremors, muscle rigidity, overactive reflexes). Symptoms usually appear within hours of a drug change or overdose. If you’re on an SSRI and triptan and suddenly develop a high fever, stiff muscles, or confusion, seek medical help - but remember, this is extremely unlikely with this combination.
Is it safe to take triptans with other antidepressants like SNRIs?
Yes. SNRIs like venlafaxine or duloxetine work similarly to SSRIs by increasing serotonin levels, and sometimes norepinephrine too. The same evidence applies: large studies show no increased risk of serotonin syndrome when triptans are used with SNRIs. The American Headache Society includes SNRIs in its recommendation to avoid unnecessary restrictions on triptan use.
Should I stop my SSRI if I want to start triptans?
No. There is no medical reason to stop your SSRI to take a triptan. Stopping an antidepressant suddenly can cause withdrawal symptoms and worsen your mood or anxiety. If your migraine is under control and your depression is stable, you can safely use both. The goal is to treat both conditions - not sacrifice one for the other.
Are there any drugs I should avoid with triptans?
Yes - but not SSRIs or SNRIs. The real danger comes from MAOIs (monoamine oxidase inhibitors), like phenelzine or selegiline. These drugs dramatically increase serotonin levels and can cause serotonin syndrome when combined with triptans. If you’re on an MAOI, you should not take triptans. Also avoid combining triptans with other strong serotonin-boosting drugs like dextromethorphan, certain opioids (tramadol, meperidine), or illicit drugs like MDMA. SSRIs and SNRIs are not in this high-risk group.





There are 14 Comments
Shannara Jenkins
Just wanted to say thank you for this post. I’ve been on sertraline for 8 years and started sumatriptan last year after my neurologist assured me it was fine. No issues. No weird symptoms. Just fewer migraine days and less anxiety about taking my meds. It’s frustrating when pharmacists act like you’re about to die from a combo that’s been used by millions.
Joel Deang
Yooo this is wild 😅 I’ve been on fluoxetine + rizatriptan for 5 years and never even thought twice. My pharmacist still flags it every time like I’m smuggling cocaine and serotonin in the same bag. Bro, the science’s been out since 2019. Update your system pls 🙏
Ella van Rij
Oh wow. A post that doesn’t end with ‘I’m not a doctor but…’? Radical. I’m shocked. Someone actually cited JAMA Neurology. Did you write this in a Harvard library or just Google Scholar for 17 minutes? 😏
Jack Dao
People like you are why medicine is broken. You read one study and suddenly you’re a neurologist? What about individual variability? What about rare cases? You’re just spreading dangerous optimism. Next you’ll say vaping is safe because one guy lived to 90.
Steve World Shopping
The pharmacodynamic profile of triptans exhibits negligible affinity for 5-HT2A receptors, thereby precluding the cascade of receptor-mediated hyperstimulation that defines serotonin toxicity. SSRIs, by contrast, inhibit SERT-mediated reuptake, yet the pharmacokinetic overlap remains non-synergistic. The FDA warning was a heuristic artifact, not a clinical imperative.
मनोज कुमार
So what? The system still blocks it. Doctors still scare patients. You think posting data fixes that? Nah. People fear what they don’t understand. You’re preaching to the choir. The problem’s not knowledge. It’s inertia.
Zed theMartian
Wow. So you’re saying the FDA got it wrong? Shocking. Next you’ll tell me cigarettes aren’t addictive or that the moon landing was faked. I mean, who are you to contradict a government agency? 😏
Arun kumar
in india most doc still say dont mix. i told my doc about this and he said ‘oh you read internet’ 😑 i just stopped asking. but i take both anyway. no problem. 3 years now. my head dont explode.
ATUL BHARDWAJ
Good post. Real data. No drama. Why is this so rare? Pharma doesn’t profit from telling people their old meds are safe. They profit from new expensive drugs. CGRP inhibitors cost $10k/year. Sumatriptan is $5. Coincidence?
Jay Everett
This is the kind of post that makes me believe Reddit still has a soul 🫡 I’ve been prescribing triptans with SSRIs since 2018. Zero cases. Zero scares. Just happy patients who can finally function. The real tragedy? The ones who suffered for years because someone’s EHR still says ‘DANGER’ in bright red. Thanks for putting the facts out there. This needs to go viral.
Elizabeth Grace
I cried reading this. I’ve been on Lexapro for 6 years and got migraines since I was 12. My last neurologist refused to give me triptans. I went to the ER three times because my migraine wouldn’t break. They gave me IV toradol and sent me home. I felt like a burden. Then I found a new doc who said ‘you’re fine’. I started sumatriptan last month. I haven’t missed work since. Thank you for saying what I needed to hear.
dave nevogt
The deeper issue here isn’t just pharmacology-it’s epistemology. We live in a culture that conflates institutional authority with truth, and algorithmic alerts with clinical wisdom. The FDA warning was a product of precautionary principle run amok, a bureaucratic overcorrection born of incomplete data and media panic. Meanwhile, real-world evidence-patient outcomes, longitudinal studies, real-time clinical observation-has been systematically ignored. The persistence of this myth reveals a systemic failure: we prioritize protocol over pragmatism, fear over freedom, and liability over lived experience. And yet, here we are: patients, doctors, pharmacists, all slowly, stubbornly, reclaiming agency from the machine. This isn’t just about serotonin receptors. It’s about who gets to decide what’s safe for your body.
Laura Baur
It’s fascinating how easily people dismiss the FDA as ‘outdated’ while ignoring the fundamental principle of medical ethics: first, do no harm. Even if the risk is low, it’s not zero. And when you have patients with comorbid anxiety, depression, and migraines-already vulnerable populations-why take any chance? What if someone’s metabolizing drugs differently? What if they’re on an undisclosed supplement? The burden of proof shouldn’t be on the patient to prove they’re safe-it should be on the prescriber to prove it’s *always* safe. This isn’t just about data. It’s about responsibility.
Rebecca M.
Oh my god I’m so relieved. I’ve been taking both for 4 years and every time I go to the pharmacy I get the side-eye like I’m trying to make a meth lab in my bathroom. I just said ‘I’m fine’ and walked out. My pharmacist now just sighs and hands me the script. I’m not a statistic. I’m a person. And I’m not dying. 😌
Write a comment
Your email address will not be published. Required fields are marked *