
Choosing between basal-bolus and premixed insulin isn’t just about numbers on a glucose meter-it’s about how your life actually works. If you’re juggling a shift job, caring for kids, or dealing with arthritis, your insulin regimen needs to fit your day, not the other way around. And the side effects? They’re not the same for everyone.
How These Two Insulin Systems Work
Basal-bolus therapy is like having two separate tools for two different jobs. One is a long-acting insulin-think of it as your background dose-that keeps your blood sugar steady between meals and overnight. The other is a fast-acting insulin you take right before eating to handle the sugar spike from food. Most people on this plan take 4 to 5 shots a day: one or two for basal, and one before each meal, sometimes with an extra dose to fix high blood sugar. Premixed insulin is simpler in packaging. It’s a fixed blend-usually 30% fast-acting and 70% intermediate-acting insulin-in one syringe or pen. You take it twice a day, typically before breakfast and dinner. There’s no splitting doses or counting carbs. You just inject, eat, and hope the mix matches your meal. The trade-off? Basal-bolus gives you control. Premixed gives you convenience. But control doesn’t always mean better outcomes if you can’t stick with it.Side Effects: Which One Risks More Low Blood Sugar?
Hypoglycemia is the biggest fear with any insulin. But the risk isn’t equal. Premixed insulin carries a higher chance of low blood sugar, especially if you skip a meal or eat less than usual. Because the fast-acting part is locked into the dose, you can’t adjust it. If you eat a light lunch, you’re still getting the full dose meant for a full meal. That’s why hospital studies in 2015 had to stop early-over half the patients on premixed human insulin had dangerous low blood sugar episodes. Basal-bolus isn’t risk-free, but it’s more forgiving. You can skip a meal without injecting the prandial dose. You can adjust your correction dose based on your current blood sugar. A 2014 meta-analysis found no statistically significant difference in overall hypoglycemia rates between the two, but that’s because the data was averaged across all patients. For those with irregular schedules, the risk with premixed insulin spikes. Real-world stories back this up. One Reddit user wrote: “I switched from premixed to basal-bolus because I couldn’t handle the rigid meal schedule-missing a meal meant risking hypoglycemia even if my blood sugar was normal.”Does One Cause More Weight Gain?
Yes, but not as much as you might think. Both types can lead to weight gain because insulin helps your body store calories. But the numbers tell a clear story: basal-bolus users gained an average of 1.9 kg over time, while premixed users gained about 1.0 kg. Why? Because basal-bolus users often take more total insulin to get tighter control. More insulin = more fat storage. But here’s the twist: if you’re using continuous glucose monitoring (CGM) and adjusting your food intake, you can offset that gain. With premixed, you’re less likely to adjust your eating habits because the insulin dose is fixed. So you might eat the same amount, get the same insulin, and gain weight without even realizing why.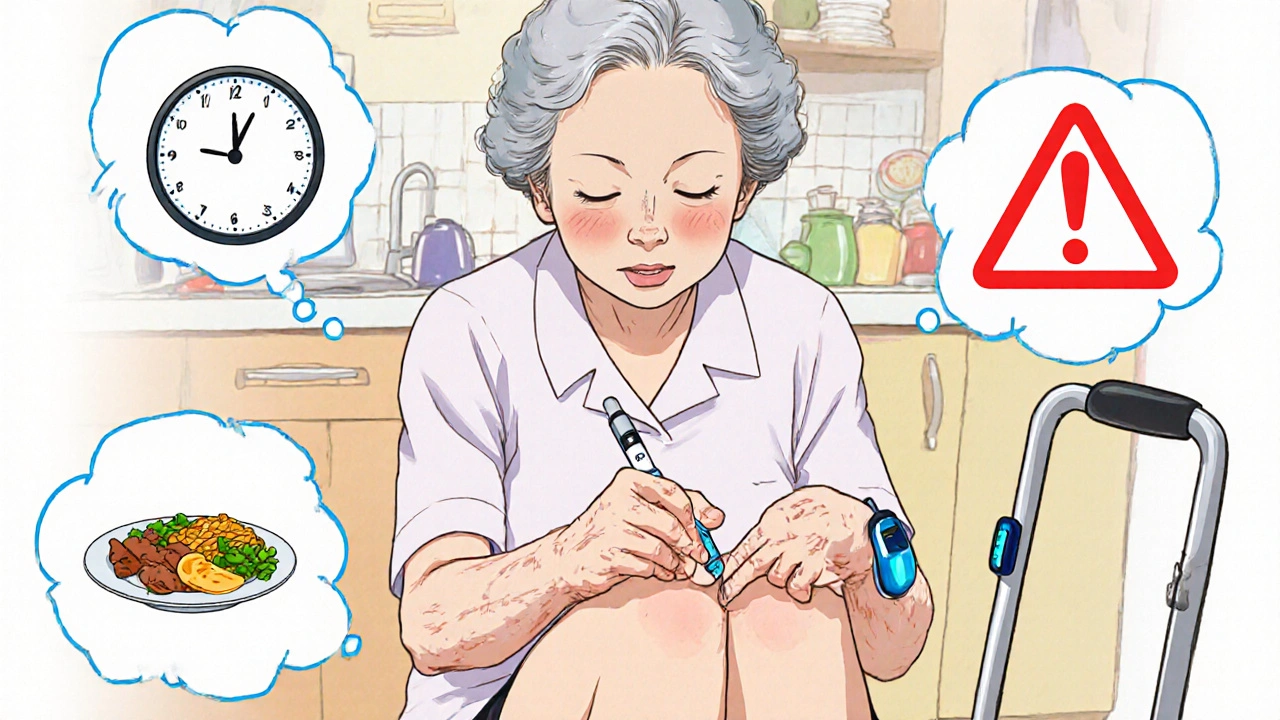
Which One Gives Better Blood Sugar Control?
Basal-bolus wins on HbA1c numbers. In the same 2014 study, 63.5% of people on basal-bolus reached an HbA1c under 7%, compared to just 50.8% on premixed insulin. That’s a big gap. The reason? Flexibility. You can fine-tune your mealtime insulin based on what you eat, how active you are, and your blood sugar before the meal. But here’s where it gets messy. Another study from 2018 found that premixed insulin actually led to better long-term control in some populations-especially older adults with type 2 diabetes who weren’t on multiple medications. Why? Because consistency beats complexity. If someone can’t remember to take four shots a day, or doesn’t understand carb counting, they’ll do better with two fixed doses-even if the numbers aren’t perfect. The key isn’t which regimen is “better.” It’s which one you can stick with.Lifestyle Fit: Flexibility vs Routine
If your life is predictable-three meals a day, same time, same portions-premixed insulin might work fine. It’s easier to learn, easier to manage, and cheaper. Medicare data shows premixed insulins cost about $45.75 a month out-of-pocket, while basal-bolus runs closer to $68.20 because you’re buying two or three separate products. But if your life is messy? Basal-bolus wins. Late-night shift? Skip the dinner shot. Spontaneous lunch? Take your fast-acting insulin and go. Traveling across time zones? Adjust your basal dose. That flexibility is priceless. One elderly patient on the ADA forum said: “Two shots a day instead of four has made managing my diabetes possible since my arthritis makes multiple injections painful.” For her, convenience outweighed perfect numbers. Basal-bolus requires skills: carb counting, understanding insulin-to-carb ratios, knowing how to correct highs, and checking your blood sugar before each meal. It’s a 8- to 12-week learning curve. Many primary care doctors still feel unprepared to teach it-only 42% say they’re confident initiating it.
Who Should Choose What?
Here’s a simple guide:- Choose basal-bolus if: You have type 1 diabetes, you eat irregular meals, you’re active or travel often, you’re comfortable with numbers and tech (like CGM), and you want the tightest control possible.
- Choose premixed insulin if: You have type 2 diabetes with stable routines, you struggle with multiple daily injections, you have limited cognitive or dexterity challenges, you’re on a tight budget, or you’re older and prefer simplicity over precision.
What’s Changing in 2025?
New tools are blurring the lines. The FDA approved a “basal-plus” insulin in 2023-a single long-acting shot you can add a fast-acting dose to only when you eat. It’s not full basal-bolus, but it’s more flexible than premixed. And then there’s tech. AI-powered insulin calculators like Diabeloop are cutting the mental load of basal-bolus. In trials, users needed 27% fewer decisions per day. CGM use is shrinking the hypoglycemia gap between regimens-people on premixed insulin with CGM now have nearly the same low blood sugar rates as those on basal-bolus. By 2030, experts predict basal-bolus will become the standard in high-income countries-not because it’s perfect, but because technology is making it easier.What If You’re Not Sure?
Talk to your diabetes educator-not just your doctor. Ask for a trial. Try basal-bolus for a month with CGM. See how you feel. Then try premixed with fixed meals for two weeks. Track your blood sugar, your energy, your stress levels. Your insulin regimen isn’t permanent. You can switch. You can change. You can start with premixed and move to basal-bolus later. Or vice versa. The goal isn’t to pick the “best” insulin. It’s to pick the one that lets you live your life without diabetes holding you back.Can I switch from premixed to basal-bolus insulin later?
Yes, switching is common and often recommended if your lifestyle changes or your blood sugar control isn’t where you want it. Many people start with premixed insulin because it’s simpler, then move to basal-bolus when they need more flexibility or better HbA1c results. Your healthcare team will adjust your doses gradually, usually over 1-2 weeks, and teach you carb counting and glucose monitoring. Don’t feel locked in-your needs can evolve.
Does basal-bolus insulin cause more weight gain than premixed?
Yes, on average, basal-bolus users gain slightly more weight-about 1.9 kg compared to 1.0 kg with premixed insulin. This is because basal-bolus typically requires higher total daily insulin doses to achieve tighter control, and insulin promotes fat storage. But weight gain isn’t inevitable. With proper nutrition coaching, carb counting, and activity, many people maintain or even lose weight while on basal-bolus. The key is matching insulin to actual food intake, not just taking it automatically.
Why do some doctors prefer prescribing premixed insulin?
Many doctors choose premixed insulin because it’s easier to teach and manage, especially in busy clinics. Only 42% of primary care providers feel confident starting basal-bolus therapy, compared to 78% for premixed. Premixed requires less patient education-no carb counting, no multiple doses. It’s also cheaper out-of-pocket. For patients with stable routines, limited health literacy, or physical challenges like arthritis, premixed can be a practical, safe choice-even if it’s not the most precise.
Is CGM enough to make premixed insulin safer?
Yes, continuous glucose monitoring (CGM) significantly reduces the hypoglycemia risk with premixed insulin. Studies show users on premixed with CGM have only 0.2 low blood sugar events per month, compared to 0.8 without CGM. CGM lets you see trends, catch drops early, and adjust meals or activity in real time. For people who prefer fewer injections but still want safety, CGM turns premixed insulin into a much more viable long-term option.
Can I use basal-bolus insulin if I have arthritis or trouble with injections?
It’s harder, but not impossible. Basal-bolus requires 4-5 daily injections, which can be tough with limited hand mobility. But modern insulin pens are lightweight, have easy-to-turn dials, and some even have voice guidance. You can also use an insulin pump, which eliminates most injections-just change the site every 2-3 days. If injections are a barrier, talk to your doctor about pump therapy or basal-plus options, which reduce the number of daily shots.
Which insulin regimen is cheaper?
Premixed insulin is usually cheaper out-of-pocket. In the U.S., Medicare Part D data shows an average monthly cost of $45.75 for premixed, compared to $68.20 for basal-bolus, because basal-bolus requires two or three separate insulin products. In countries like India and parts of Asia, premixed insulin makes up over half of prescriptions because it’s more affordable and accessible. But if you’re on insurance with good coverage, the cost difference may be minimal. Always check your pharmacy’s pricing-sometimes generic basal insulins like NPH are very affordable.






There are 11 Comments
Malia Blom
Look, I get that basal-bolus sounds fancy with all your CGM stats and insulin-to-carb ratios, but let’s be real-most people don’t live in a lab. I work nights, feed my kid at 2 a.m., and sometimes eat cold pizza at 6 a.m. because why not? Premixed lets me just inject and go. No math. No stress. My HbA1c’s 7.1 and I’m not dying. Stop acting like control equals virtue when it just equals more injections and anxiety. 🤷♀️
Erika Puhan
It’s statistically indefensible to promote basal-bolus as the gold standard without acknowledging the systemic bias toward technocratic solutions in Western medicine. The data you cite is cherry-picked from high-income, digitally literate cohorts. In India, where 70% of diabetics are self-managed with minimal education, premixed insulin remains the only viable option-not out of preference, but out of necessity. To equate flexibility with superiority is a colonial mindset dressed in endocrinology jargon.
Edward Weaver
Ugh, another ‘it’s about lifestyle’ post. Newsflash: America doesn’t have time for your excuses. If you can’t handle four shots a day, maybe you shouldn’t be on insulin at all. We’ve got people in the military managing insulin on deployment with zero tech. You want convenience? Get a job. Stop blaming your laziness on your pancreas. Basal-bolus is the only real option for adults who want to live. Period.
Lexi Brinkley
Okay but can we just talk about how CGM is literally a game changer?? 🤯 I was on premixed and had 3 lows a week. Got a Dexcom, now I’m stable AF. No more panic attacks before lunch. Also, insulin pens are SO much easier now-my grandma uses one with voice prompts. 🙌 It’s not about the regimen, it’s about the tools. Tech is the real MVP.
Kelsey Veg
premixed is for people who cant spell carb counting and dont wanna think. basal-bolus is for adults. if you cant do 4 shots a day, maybe you shudnt be diabetic. also why do people think insulin = weight gain? its not the insulin its the donuts. duh.
Alex Harrison
I switched from premixed to basal-bolus last year after my doc pushed me. Honestly? It was rough at first. I messed up doses, got scared of lows, forgot to check before snacks. But after 3 months, I started feeling like myself again-more energy, less brain fog. I still mess up sometimes, but the freedom to skip a meal or eat sushi at midnight? Worth it. Just give yourself time. And get a good educator. They’re not just a nurse-they’re your diabetes coach.
Jay Wallace
Let’s not romanticize ‘lifestyle fit’-this isn’t a spa retreat, it’s a chronic disease. The ADA says ‘individualized,’ but individualized doesn’t mean ‘whatever’s easiest.’ Basal-bolus is the only regimen that reflects physiological reality. Premixed is a Band-Aid on a hemorrhage. If you’re too ‘busy’ or ‘tired’ to manage it, you’re not ready for insulin. And if your doctor is too lazy to teach you, find a new one. This isn’t 1998 anymore.
Alyssa Fisher
There’s something deeply human about this conversation. We’re not just talking about insulin-we’re talking about dignity. The ability to eat when you’re hungry, to sleep when you’re tired, to live without being ruled by a clock. Premixed insulin isn’t failure-it’s adaptation. Basal-bolus isn’t superiority-it’s privilege. The real question isn’t which is better, but who gets to decide what ‘better’ means. And why do we assume that those who need simplicity are less capable? Maybe the problem isn’t the patient. Maybe it’s the system.
Alyssa Salazar
Let’s cut through the noise: basal-bolus has higher hypoglycemia risk in real-world settings because people skip meals, forget doses, or miscount carbs. Premixed has lower variability because it’s predictable. That’s not laziness-that’s pharmacokinetics. And yes, CGM reduces risk, but it doesn’t eliminate human error. The goal isn’t perfect HbA1c-it’s sustainable safety. If you’re not measuring outcomes by quality of life, you’re not measuring at all.
Beth Banham
I’ve been on premixed for 8 years. My hands shake from arthritis, and I can’t hold a pen anymore. I don’t care about HbA1c numbers as long as I’m not in the ER. My insulin pen has a big dial. I press the button. I eat. I live. That’s enough. I’m not here to win a science fair. I’m here to watch my grandkids grow. And I’m not going to let anyone make me feel less because I chose peace over precision.
Brierly Davis
Hey everyone-just want to say this: you’re all right. Some of you need flexibility, some need simplicity, some need tech, some need peace. There’s no one-size-fits-all, and that’s okay. I’ve seen patients switch back and forth multiple times. It’s not a life sentence. Talk to your diabetes educator. Try a trial. Use CGM if you can. You’re not failing if it’s hard. You’re just human. And you’re doing better than you think. 💪
Write a comment
Your email address will not be published. Required fields are marked *