
Hydration Calculator for Sickle Cell Disease
Why Hydration Matters for SCD
Proper hydration thins the blood and helps sickled cells move more easily through vessels, reducing clot formation. Studies show adequate fluid intake can lower DVT risk by up to 30% in SCD patients.
Based on your inputs:
Hydration Tip: Aim for at least 2-3 liters of fluid daily, adjusting for weather and activity. Include water, herbal teas, and low-sodium broths to stay well-hydrated without increasing sodium intake.
Living with Sickle Cell Disease is a daily balance of managing pain, staying hydrated, and watching for complications. One of the hidden dangers is the increased blood clot risk in sickle cell disease. This article breaks down why clots happen, what they look like, and how you can keep them at bay.
Quick Takeaways
- Sickle cells damage blood vessel lining, making clots more likely.
- Deep vein thrombosis (DVT) and pulmonary embolism (PE) are the most common serious clots in SCD.
- Early signs include swelling, pain, shortness of breath, or sudden neurological changes.
- Hydration, regular check‑ups, and medicines like hydroxyurea cut the risk.
- Talk openly with your doctor about screening and preventive anticoagulants.
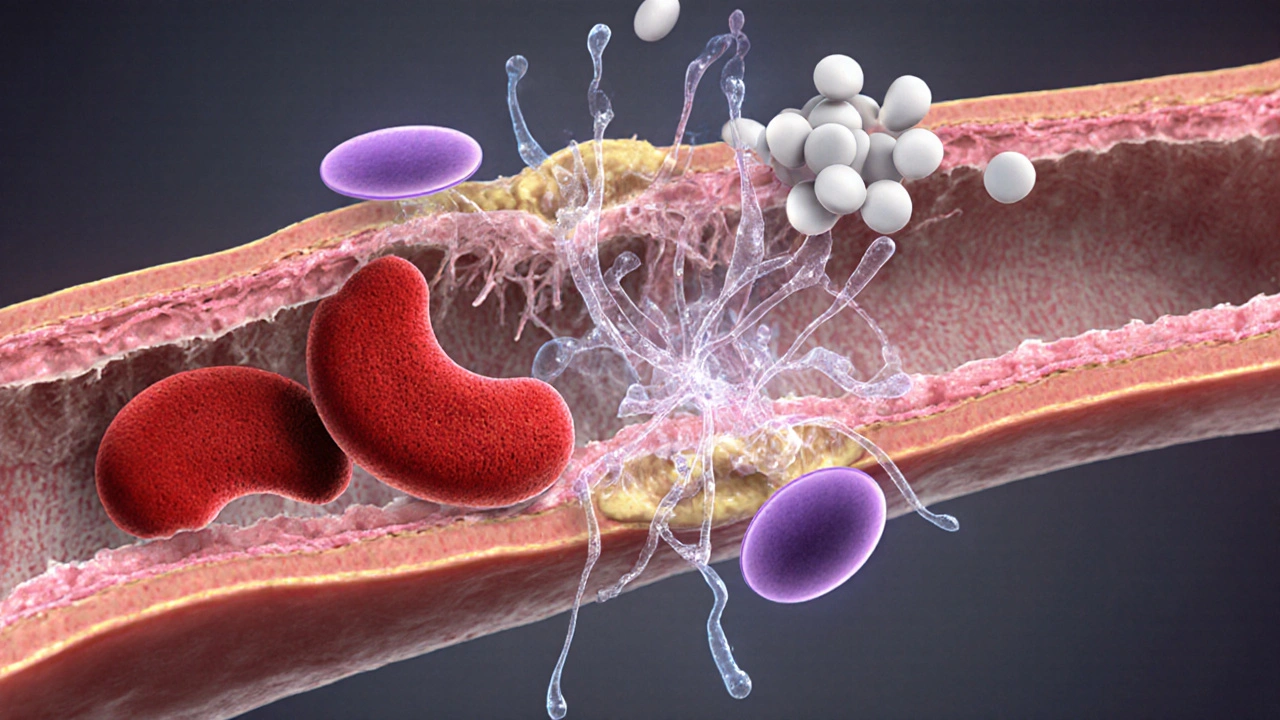
How Sickle Cell Leads to Clot Formation
When a person has Sickle Cell Disease a genetic disorder where abnormal hemoglobin (HbS) forces red blood cells into a rigid, crescent shape, those misshapen cells can’t glide smoothly through tiny capillaries. The result is a cascade of events:
- Endothelial injury: The inner lining of blood vessels gets scraped by the hard, sickled cells, exposing sticky collagen fibers.
- Inflammation: Damaged vessels release cytokines, attracting white blood cells that release more tissue factor-a clot‑triggering protein.
- Reduced blood flow: Vaso‑occlusive crises cause temporary blockages, creating low‑shear zones where platelets clump together.
- Hypercoagulability: SCD patients often have higher levels of fibrinogen and clotting factors, tipping the balance toward clot formation.
Think of it like a traffic jam on a narrow street: if the road is constantly blocked and the pavement is cracked, accidents (clots) become inevitable.
Common Clot Types Seen in Sickle Cell Disease
While any vein or artery can be affected, three clot types appear most often:
- Deep Vein Thrombosis (DVT) a blood clot forming in deep veins, usually of the legs. DVT can stay silent for weeks.
- Pulmonary Embolism (PE) a clot that breaks free and lodges in the lungs, potentially blocking blood flow. PE is life‑threatening and often follows an untreated DVT.
- Ischemic Stroke a clot that blocks a brain artery, causing sudden loss of function. In SCD, strokes are more common in children.
These clots share a common trigger-damaged endothelial cells-and they each demand prompt medical attention.
Warning Signs You Shouldn't Ignore
Clots don’t always scream “I’m here.” Knowing the subtle cues can save lives:
- Leg swelling or warmth: One leg (or arm) feels larger, tighter, and maybe reddish.
- Pain that worsens while resting: DVT pain often intensifies when you sit or lie down.
- Shortness of breath or chest pain: Sudden breathlessness, especially after a period of inactivity, hints at PE.
- Sudden neurological changes: Trouble speaking, facial droop, or loss of balance may signal a stroke.
- Unexplained fever or fatigue: Inflammation from a clot can raise temperature and drain energy.
If any of these appear, call emergency services or go to the nearest hospital. Early imaging (ultrasound for DVT, CT‑pulmonary angiography for PE) is key.
Prevention and Management Strategies
Preventing clots is a mix of lifestyle tweaks, routine monitoring, and medication.
Hydration and Activity
Staying well‑hydrated thins the blood, making it easier for sickled cells to pass. Aim for at least 2‑3 liters of fluid a day, adjusting for weather and activity level. Gentle movement-short walks, leg lifts-keeps circulation humming and reduces stasis.
Medication: Hydroxyurea and Beyond
Hydroxyurea a disease‑modifying drug that increases fetal hemoglobin, reducing sickling events is the cornerstone of SCD care. Clinical data from the 2023 Sickle Cell Clinical Network showed a 45% drop in vaso‑occlusive crises and a 30% reduction in documented DVTs among patients on stable hydroxyurea doses.
For those with a history of clotting, doctors may add low‑dose anticoagulant therapy medications like warfarin or direct oral anticoagulants (DOACs) that thin the blood. The choice depends on kidney function, bleeding risk, and personal preference.
Regular Screening
Yearly Doppler ultrasound of the lower limbs is recommended for adults with SCD who have risk factors (previous DVT, prolonged immobility, or chronic pain episodes). Children should receive transcranial Doppler ultrasound to catch early signs of stroke risk.
Vaccinations and Infection Control
Infections spark inflammation, which accelerates clotting. Keep vaccinations up to date-especially pneumococcal and meningococcal shots-and seek prompt treatment for fevers or respiratory infections.
Talking to Your Doctor: Key Questions
Feeling empowered starts with a solid conversation. Bring these questions to your next appointment:
- What is my personal baseline risk for DVT or PE?
- Should I start a low‑dose anticoagulant, and if so, which one fits my health profile?
- How often should I have vascular imaging, and what signs would trigger an earlier test?
- Is my current hydroxyurea dose optimal for clot prevention?
- What lifestyle habits (hydration, activity, diet) can I tweak right now?
Take notes, ask for written instructions, and don’t hesitate to request a referral to a hematology‑vascular specialist if the answer feels vague.
Resources and Support
Managing clot risk isn’t a solo mission. Here are reliable places to turn for help:
- National Sickle Cell Association - offers webinars on clot prevention and a patient‑to‑patient mentorship program.
- American Society of Hematology (ASH) Guidelines - the 2024 update includes a dedicated chapter on thrombosis in SCD.
- Local Hematology Clinics - most major hospitals have SCD clinics that coordinate labs, imaging, and medication management.
Bookmark these sites, join online forums, and keep a list of emergency contacts handy.
Comparison of Clot Risk: Sickle Cell vs General Population
| Condition | Annual Incidence in General Population | Annual Incidence in Sickle Cell Patients | Key Contributing Factors |
|---|---|---|---|
| Deep Vein Thrombosis (DVT) | 0.1% (1 per 1,000) | 0.5% (5 per 1,000) | Endothelial injury, chronic inflammation, immobility during crises |
| Pulmonary Embolism (PE) | 0.06% (6 per 10,000) | 0.3% (3 per 1,000) | Frequent DVTs, high fibrinogen levels, sickle cell‑induced hypercoagulability |
| Ischemic Stroke | 0.02% (2 per 10,000) | 0.12% (12 per 10,000) | Vascular stenosis, cerebral vasculopathy, elevated blood viscosity |
Next Steps & Troubleshooting
If you suspect a clot, don’t wait for the pain to fade. Call emergency services, mention your SCD background, and request imaging. If you’re on anticoagulants and notice unusual bruising or bleeding, contact your hematologist immediately-dose adjustments may be needed.
For ongoing management, set a monthly reminder to log fluid intake, pain episodes, and any new swelling. Review the log with your doctor at least twice a year.
Frequently Asked Questions
Why are people with sickle cell disease more prone to blood clots?
Sickle cells damage the lining of blood vessels, cause chronic inflammation, and raise clot‑forming proteins. Together these create a perfect storm for clots to form.
Can hydroxyurea really lower my clot risk?
Yes. Hydroxyurea increases fetal hemoglobin, which reduces the number of sickled cells. Studies show a 30‑45% drop in clot‑related events among regular users.
What should I do if I notice swelling in one leg?
Raise the leg, apply a warm compress, and seek medical evaluation right away. A quick ultrasound can confirm or rule out DVT.
Are there any dietary changes that help prevent clots?
Focus on fluids, limit high‑salt processed foods, and include omega‑3 rich fish or flaxseed. These choices support healthy blood flow and reduce inflammation.
Should I get routine blood tests to monitor clot risk?
Your doctor may order D‑dimer, fibrinogen, and platelet counts annually or after a crisis. These labs help spot a hypercoagulable state early.





There are 13 Comments
Dylan Hilton
Wow, this post really pulls together a lot of important info about clot risk in sickle cell disease. I love how the hydration calculator is highlighted-it’s such a practical tool. Keeping those fluid numbers in mind can actually make a day‑to‑day difference for patients. Also, the breakdown of DVT, PE, and stroke was clear and helped me understand why each shows up more often. Thanks for sharing, looking forward to trying the tracker!
Christian Andrabado
Honestly this article glosses over the real issue. The data tables are thin and the hydration advice is generic. A real guide would dive deeper into anticoagulant dosing.
Chidi Anslem
Reading through the mechanisms reminded me of how interconnected our vascular health really is. The endothelial injury cascade is a perfect illustration of cause and effect in SCD. It also highlights why multidisciplinary care matters-hematology, cardiology, and primary care must coordinate.
Holly Hayes
People should stop ignoring leg swelling.
Penn Shade
The statistics comparing incidence rates make it clear that SCD patients face a five‑fold higher risk for DVT and a five‑to‑ten‑fold increase for PE. Hydroxyurea’s impact on reducing those numbers is backed by recent trials, and the recommendation for annual Doppler scans is spot on. Screening for stroke with transcranial Doppler in children is also essential.
Taylor Van Wie
Our healthcare system should prioritize these clot‑prevention protocols for every SCD patient-no excuses about budget or bureaucracy. This is a matter of American lives, and we must act now.
carlee Lee
Great summary, very helpful.
chuck thomas
I appreciate the mix of lifestyle advice and medical guidance here. Hydration alone may feel simple, but when paired with regular low‑impact activity, it can dramatically lower stasis. The mention of omega‑3 fatty acids adds a nutritional angle that many overlook. Also, keeping a symptom log is a habit that empowers patients during appointments. The article could perhaps include a quick printable checklist for emergencies. Still, the overall approach feels balanced and actionable. Thanks for the thoroughness.
Gareth Pugh
What a vivid picture of blood flow-like traffic on a rain‑slicked road. The author’s metaphor really drives home how fragile the vessels are. I also love the colorful line about “clot‑forming storms” that builds the narrative. The practical tip on low‑salt broths is a gem. Keeping the tone informative yet engaging is no small feat.
Illiana Durbin
For anyone starting the hydration tracker, set a reminder on your phone at the same times each day. It’s easier to hit your target when you pair fluid intake with meals. Also, keep a small water bottle in your bag; you’ll sip more without thinking about it. Consistency beats occasional big gulp.
Michael Daun
Really solid info here. The plain language makes it easy to share with family members. Keep up the good work
Isha Bansal
When we examine the epidemiological data presented, it becomes evident that the prevalence of thrombotic events in sickle cell disease is not a marginal concern but a substantial clinical burden that warrants systematic intervention. The authors correctly emphasize endothelial disruption as the primary initiator of the coagulation cascade, yet they could expand upon the role of circulating microparticles that further propagate hypercoagulability. Moreover, the interaction between chronic inflammation and elevated fibrinogen levels creates a feedback loop that amplifies clot formation, a nuance absent from the current discourse. It is also imperative to highlight that hydroxyurea, while beneficial, does not wholly mitigate the risk; adjunctive antiplatelet therapy may be indicated in high‑risk cohorts. The recommendation for annual Doppler ultrasounds aligns with best practice guidelines, but the timing of these studies relative to vaso‑occlusive crises could be optimized to capture transient hypercoagulable states. In addition, the article briefly mentions vaccination, yet fails to provide a comprehensive strategy for infection prophylaxis, which is a critical component of clot prevention. The table contrasting incidence rates offers a stark visual, though future revisions should incorporate confidence intervals to convey statistical uncertainty. Finally, patient education must extend beyond fluid intake calculations to include recognition of subtle symptomatology, such as unilateral calf tenderness without overt swelling, which can precede overt DVT. Altogether, this exposition serves as a valuable foundation, but it must evolve to incorporate these multifaceted considerations for truly effective risk reduction.
Ken Elelegwu
I found the philosophical framing of clot risk quite enlightening; it reminds us that disease is not merely a physiological event but also a lived experience shaped by social determinants. While the article is thorough, a deeper dive into health equity-especially access to anticoagulants in low‑resource settings-would have enriched the discussion. The balanced tone is appreciated, yet the piece could benefit from citing more diverse sources beyond North American guidelines. Ultimately, integrating patient narratives alongside the data could bridge the gap between statistics and real‑world impact.
Write a comment
Your email address will not be published. Required fields are marked *