
When someone takes too much of a sedative or sleep medication, they don’t just fall into a deep sleep-they can stop breathing. And if no one notices, they may not wake up. This isn’t rare. In 2021, over 12,500 people in the U.S. died from benzodiazepine overdoses alone. Many of these deaths happened because the warning signs were missed-written off as just being "really tired" or "drunk." But the difference between sleep and overdose is life or death.
What Counts as an Overdose?
An overdose happens when the body can’t handle the amount of drug in the system. Sedatives and sleep meds like zolpidem (Ambien), eszopiclone (Lunesta), temazepam (Restoril), and alprazolam (Xanax) slow down your brain and nervous system. That’s why they help you sleep. But too much? It shuts down your breathing.It’s not just prescription drugs. Over-the-counter sleep aids like diphenhydramine (Benadryl, Tylenol PM) can also cause overdose. People think, "It’s just an antihistamine," but at high doses, it can cause seizures, hallucinations, and heart rhythm problems.
And here’s the real danger: mixing these with alcohol or opioids. That’s when things go from bad to deadly fast. The CDC says 23% of benzodiazepine overdose deaths in 2021 also involved fentanyl. The two together crush your breathing faster than either drug alone.
The Clear Signs of Overdose
There’s a pattern. It doesn’t come out of nowhere. It starts slow and gets worse fast. Here’s what to watch for:- Unresponsive - Shout their name. Shake their shoulder. Try a sternal rub (rub your knuckles hard on the center of their chest). If they don’t react at all, that’s a red flag. They’re not sleeping. They’re unconscious.
- Slow or shallow breathing - Count breaths for 30 seconds. Normal is 12-20 per minute. Below 8? That’s emergency territory. Breathing may be so shallow you can’t see the chest rise. This is the #1 killer in sedative overdoses.
- Cyanosis - Lips, fingertips, or nails turning blue or gray. That means oxygen is dropping below 90%. Skin may also feel cold and clammy.
- Slurred speech - Words come out like they’re drunk. This happens in 87% of benzodiazepine overdoses, even if they haven’t had alcohol.
- Loss of coordination - Can’t stand, walk straight, or hold a cup. Movements are clumsy, uncontrolled. This is called ataxia. It’s in 76% of cases.
- Confusion or memory loss - They don’t know where they are. Can’t remember what happened 10 minutes ago. This isn’t just being tired. It’s brain function shutting down.
- Heart rate and temperature drop - Pulse below 50 beats per minute. Body temperature below 95°F (35°C). This means the body is entering a critical state.
Some people think, "They’re just passed out." But passed out from alcohol? That’s different. Sedative overdose doesn’t wake up with coffee or fresh air. It gets worse. And fast.
What Doesn’t Look Like an Overdose
Not every sleepy person is overdosing. Here’s what’s usually safe:- Melatonin - Even at 240mg (60 times the normal dose), it causes headaches and dizziness, not breathing problems. It’s not a CNS depressant like prescription drugs.
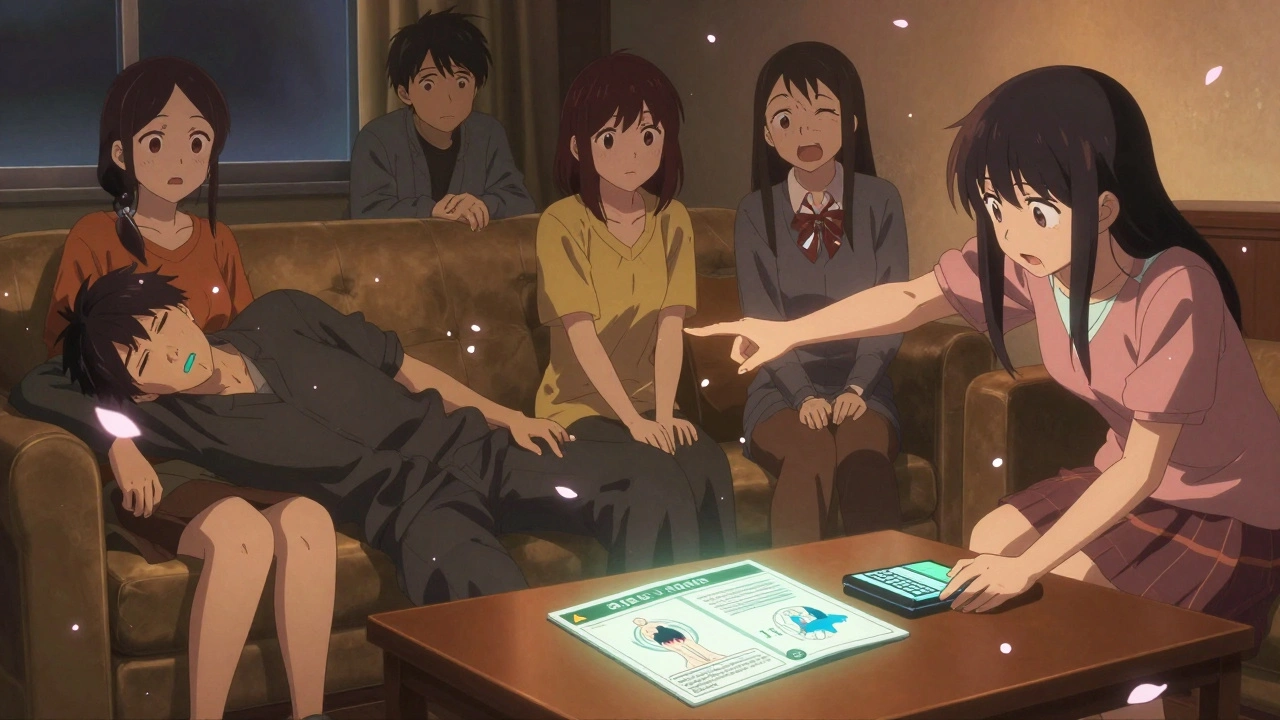
- Just being tired - If someone falls asleep on the couch after a long day, they’ll still respond to loud noises or a gentle shake. They’ll wake up if you call their name.
- Drinking alcohol alone - While alcohol can make you drowsy, you usually still react to stimuli. Overdose means no reaction at all.
But don’t rely on guesswork. If you’re unsure, assume it’s an overdose. Better to call for help than wait.

Why People Miss the Signs
A 2022 study of over 1,200 sedative overdose cases found that 68% of bystanders thought the person was just "deep asleep." They waited. They hoped they’d wake up. The average delay before calling 911? 47 minutes.Reddit threads from r/OverdoseHelp are full of stories like:
- "I thought my roommate was just exhausted from work. I left him alone for two hours. When I checked, he wasn’t breathing."
- "He was slurring his words, so I assumed he’d been drinking. I didn’t know he was on Ambien."
These aren’t careless people. They’re loved ones who didn’t know what to look for. That’s why recognition matters more than ever.
What to Do If You Suspect an Overdose
There’s no time to wait. Follow this simple checklist:- Check responsiveness - Shout their name. Shake them. Do a sternal rub. If no response, move to step two.
- Check breathing - Look at their chest. Count breaths for 30 seconds. Multiply by two. If it’s below 12, act now.
- Check for blue lips or cold skin - These mean oxygen is failing.
- Call emergency services immediately - Even if they’re breathing, call 911. Don’t wait for them to get worse.
- Start rescue breathing if they’re not breathing - Tilt their head back, pinch the nose, give one breath every 5 seconds. Don’t stop until help arrives.
- Do NOT give them flumazenil - It’s a reversal drug, but only for hospitals. Giving it at home can trigger seizures, especially if they’ve been taking sedatives regularly.
- Stay with them - Don’t leave them alone. Monitor breathing. Keep them on their side if they’re vomiting to prevent choking.
Every minute counts. Research shows survival drops 7-10% for every minute without help after breathing stops.
What Makes It Worse
Some situations raise the risk dramatically:- Combining with alcohol - This happens in 41% of fatal overdoses.
- Combining with opioids - Fentanyl mixed with benzodiazepines is a deadly combo. The CDC says this combination has driven the biggest spike in overdose deaths since 2015.
- Using multiple prescriptions - Someone taking Xanax from one doctor and Ambien from another is at high risk. Doctors don’t always know what else you’re on.
- Using old prescriptions - People keep old pills "just in case." But tolerance changes. A dose that was safe last year can kill now.
Look around the room. Are there empty pill bottles? Multiple prescriptions? Empty liquor bottles? These are clues. Don’t ignore them.
Who’s at Highest Risk?
Data shows:- People aged 25-54 are most affected.
- West Virginia has the highest overdose rate in the U.S. at 3.8 deaths per 100,000 people.
- 9.5 million Americans misused prescription sedatives in 2021.
- 58% of overdoses happen at home - where no one is trained to respond.
It’s not just "addicts." It’s people with anxiety, insomnia, chronic pain. People who took their meds as prescribed but accidentally doubled up. People who drank a glass of wine with their pill. People who thought, "One more won’t hurt."
What’s Changing Now
New tools are helping:- Wearable pulse oximeters - Devices that track oxygen levels can warn of dropping levels before breathing stops. Johns Hopkins research shows they can give 15-20 minutes of early warning.
- Overdose recognition cards - California distributed 250,000 cards to pharmacies. They show pictures of the key signs. Early results show a 22% increase in bystander recognition.
- Emergency nasal sprays - Drugs like nayzilam are now approved for use by paramedics to quickly reverse seizures or severe sedation.
But none of this matters if you don’t know what to look for.
Final Reminder
You don’t need to be a doctor to save a life. You just need to know the signs and act fast.If someone is unresponsive, breathing fewer than 12 times a minute, or has blue lips - call 911. Right now. Don’t wait. Don’t try to wake them with cold water. Don’t put them in a shower. Don’t assume they’ll sleep it off.
They’re not sleeping. They’re dying.
Know the signs. Act fast. Save a life.






There are 8 Comments
Steve Sullivan
George Taylor
ian septian
Chris Marel
Andrea Petrov
Iris Carmen
Suzanne Johnston
Carina M
Write a comment
Your email address will not be published. Required fields are marked *