
Every year, thousands of people end up in the hospital because of something they thought was harmless: a daily painkiller. NSAIDs - like ibuprofen, naproxen, and even low-dose aspirin - are everywhere. You can buy them over the counter. Your neighbor takes one for arthritis. Your parent swallows one every morning for heart health. But what if that daily pill is quietly damaging your gut? And what happens when you take too much?
The truth is simple: NSAID overdose isn’t just about taking a handful of pills at once. It’s often about taking the right dose, every day, for months or years - and never realizing the damage building inside you. The biggest danger? Gastrointestinal bleeding. And it doesn’t always come with warning signs.
How NSAIDs Damage Your Gut
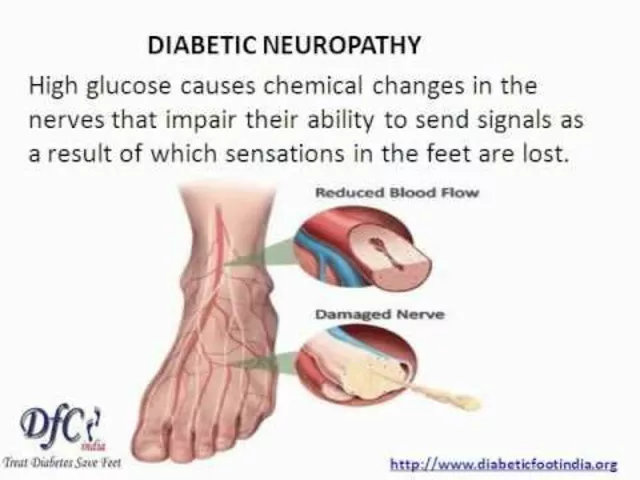
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 helps with pain and inflammation. COX-1 protects your stomach lining. When you block COX-1, you take away your body’s natural defense against stomach acid. That’s why even short-term use can cause irritation. Long-term use? That’s when things get serious.
Studies show up to 70% of people who take NSAIDs regularly have visible damage in their stomach and intestines - erosions, ulcers, even bleeding - even if they feel fine. Only about 10% report symptoms like heartburn or nausea. That means for every person who says, "I’m fine," there are six others with internal damage they don’t know about.
This isn’t just about the stomach. NSAIDs harm the entire digestive tract - from the esophagus down to the colon. They can cause bleeding in the small intestine, which is harder to detect than bleeding in the stomach. That’s why some people end up with iron-deficiency anemia without ever vomiting blood or passing black stools.
The Silent Bleeding Problem
Most people think of GI bleeding as sudden - vomiting blood, passing dark, tarry stools. But in NSAID users, bleeding is often slow and hidden. It leaks a little at a time. Your body loses iron. Your hemoglobin drops. You get tired. Your skin turns pale. You think you’re just getting older… or stressed… or not sleeping well.
Research shows over half of NSAID users who become anemic show no sign of bleeding on endoscopy. No ulcer. No lesion. Just a slow, steady loss of blood you can’t see. And because it’s silent, it’s deadly. By the time someone feels weak enough to go to the hospital, they may already be in critical condition.
One study found that over one-third of patients admitted for GI bleeding were using over-the-counter low-dose aspirin - the kind many take "just for heart health." They didn’t think it was dangerous. They were wrong.
Who’s at Highest Risk?
Not everyone who takes NSAIDs bleeds. But some people are far more vulnerable.
- People over 65: Age weakens the stomach lining. Dose matters too - taking 300 mg of aspirin daily triples your bleeding risk compared to 75 mg.
- Those with past ulcers or bleeding: If you’ve had a GI bleed before, your chance of another one while on NSAIDs is 5 times higher than someone who hasn’t.
- People on blood thinners: Combining NSAIDs with aspirin, clopidogrel, or warfarin doesn’t just add risk - it multiplies it. Taking NSAIDs with dual antiplatelet therapy (like aspirin + clopidogrel after a heart attack) doubles your chance of GI bleeding.
- People with H. pylori infection: This common stomach bacteria doesn’t just cause ulcers - it teams up with NSAIDs to make bleeding 1.2 times more likely.
- Those taking multiple NSAIDs: Taking ibuprofen and naproxen together? Or using an OTC painkiller while also on a prescription NSAID? That’s a recipe for disaster.
Here’s the scary part: many people don’t even know they’re in this high-risk group. They think, "I’m healthy. I just take a pill." But health isn’t about how you feel today - it’s about what’s happening inside you right now.

Aspirin Isn’t Safe Just Because It’s Low-Dose
Low-dose aspirin (75-100 mg) is often prescribed to prevent heart attacks. But it’s still an NSAID. And it still damages the gut.
Studies show aspirin alone increases the risk of upper GI bleeding by 2 to 4 times. That risk climbs with dose: 75 mg = 2.3x higher risk. 150 mg = 3.2x. 300 mg = 3.9x. There’s no "safe" dose - just less dangerous ones. Experts agree: stick to 81 mg if you’re on aspirin long-term. Going higher gives no extra heart protection - only more bleeding.
And don’t be fooled by "enteric-coated" or "buffered" aspirin. They don’t reduce bleeding risk. They just make the pill easier to swallow. The damage still happens.
What About COX-2 Inhibitors? Are They Safer?
Drugs like celecoxib (Celebrex) were marketed as "stomach-friendly" NSAIDs. They block COX-2 without touching COX-1. Sounds perfect, right?
Turns out, they’re not the magic solution. In people taking aspirin, COX-2 inhibitors offer no extra protection. One study found the risk of upper GI events was 5.6% per year for aspirin + traditional NSAID users - and 7.5% for aspirin + COX-2 inhibitor users. That’s not safer. That’s worse.
So if you’re on aspirin for heart health and also need pain relief, switching to a COX-2 inhibitor won’t help. You still need real protection.
What Can You Do? Prevention Is Key
There’s no cure for NSAID-induced bleeding once it starts. But it’s almost always preventable.
- Ask your doctor: Do you really need this NSAID? Is there an alternative? Physical therapy? Acetaminophen? Cold packs? Sometimes, the best treatment isn’t a pill.
- Use the lowest dose for the shortest time: Don’t take ibuprofen daily for back pain unless your doctor says it’s necessary. Try taking it only on bad days.
- Never mix NSAIDs: No combining ibuprofen, naproxen, aspirin, or celecoxib. Even if they’re "different brands," they’re the same drug.
- Get tested for H. pylori: If you’ve had ulcers or are on long-term NSAIDs, ask for a breath or stool test. Treating this infection cuts bleeding risk.
- Use a PPI if you’re high-risk: If you’re over 65, have a history of ulcers, or are on blood thinners, your doctor should prescribe a proton pump inhibitor (like omeprazole) alongside your NSAID. It doesn’t fix everything - especially not in the small intestine - but it cuts upper GI bleeding risk by 60-70%.
- Watch for hidden signs: Unexplained fatigue, pale skin, shortness of breath, or dark stools? Get your hemoglobin checked. Don’t wait for vomiting blood.
What If You’ve Already Taken Too Much?
If you took a single large overdose - say, 10+ ibuprofen tablets - go to the ER. Don’t wait. Even if you feel fine, liver and kidney damage can develop hours later.
If you’ve been taking NSAIDs daily for months and now feel tired, dizzy, or notice dark stools - see your doctor. Don’t just stop the pills. You need tests: a blood count, iron levels, and possibly an endoscopy. Stopping the NSAID is step one. Finding the damage is step two.
Never stop aspirin on your own if you’re on it for heart protection. Talk to your doctor. They may switch you to a safer painkiller or adjust your regimen.
Why This Isn’t Just a "Drug Problem"
This isn’t about bad choices. It’s about misinformation.
We’re told aspirin is "good for the heart." We’re told ibuprofen is "safe if you don’t take too much." We’re told, "It’s just a painkiller." But the science is clear: these drugs are not harmless. They’re powerful chemicals with real, measurable risks - especially when used without oversight.
The solution isn’t to avoid NSAIDs completely. It’s to use them with awareness. To treat them like prescription drugs - even when they’re sold over the counter.
Millions of people live with chronic pain. They need relief. But they also need to live. That means knowing when to reach for a pill - and when to reach for a doctor instead.
Can NSAID overdose cause death?
Yes. While a single large overdose can cause kidney failure or seizures, the bigger threat is long-term use leading to hidden GI bleeding. When bleeding goes unnoticed, it can lead to severe anemia, organ failure, or cardiac events - especially in older adults. Studies estimate NSAID-related GI toxicity causes about 0.22% of deaths per year in high-risk groups like rheumatoid arthritis patients - but because millions use these drugs, the total number of preventable deaths is substantial.
Is it safe to take ibuprofen with aspirin?
No. Taking ibuprofen with aspirin, even low-dose, significantly increases your risk of GI bleeding - by 2 to 4 times. Ibuprofen can also interfere with aspirin’s heart-protective effect. If you need both, talk to your doctor. They may advise taking aspirin first, waiting 30 minutes, then taking ibuprofen - or switching to a safer alternative like naproxen (which has less interference) or acetaminophen.
Do enteric-coated or buffered NSAIDs reduce bleeding risk?
No. These formulations are designed to reduce stomach irritation or make pills easier to swallow, but they don’t prevent damage to the gut lining or reduce bleeding risk. The mechanism of injury is still the same: blocking protective enzymes. Studies confirm enteric-coated aspirin carries the same bleeding risk as regular aspirin.
Can I take NSAIDs if I’ve had a heart attack?
Avoid NSAIDs entirely if you’re on dual antiplatelet therapy (like aspirin + clopidogrel) after a heart attack. NSAIDs raise the risk of both GI bleeding and another heart event. For pain relief, acetaminophen (paracetamol) is the safest option. If you must use an NSAID, talk to your cardiologist - they may recommend the lowest possible dose for the shortest time, and always with a PPI.
What’s the best way to check for hidden GI bleeding?
The most reliable test is a blood test for hemoglobin and ferritin (iron stores). If your hemoglobin is low and you’re on NSAIDs, further testing is needed. A fecal occult blood test can detect hidden blood in stool. For people with risk factors, an upper endoscopy (OGD) or capsule endoscopy (to check the small intestine) may be recommended. Don’t wait for symptoms - if you’re on long-term NSAIDs, ask your doctor about screening.
Final Thought: Pain Isn’t Worth the Price
NSAIDs are powerful tools. But they’re not candy. They’re not harmless. And they’re not risk-free - especially when used without understanding the cost.
The next time you reach for that bottle of ibuprofen, ask yourself: Do I really need this? Am I taking it because I’m in pain - or because I’m used to it? Have I talked to my doctor about the risks? Are there safer ways to manage this?
Because the gut doesn’t scream before it breaks. And by the time it does, it might be too late.




There are 10 Comments
PAUL MCQUEEN
Look, I get it-NSAIDs are everywhere. But let’s be real: if you’re taking ibuprofen every day for ‘back pain,’ you’re not managing pain, you’re masking it. Your body’s screaming for a reason. Physical therapy, stretching, even a damn posture correction pillow? Those are real solutions. Pills just buy you time until the next problem shows up. And don’t even get me started on people popping aspirin like M&Ms because their uncle said it ‘thins the blood.’ Bro, that’s not a vitamin. It’s a drug with side effects that don’t show up until you’re bleeding internally and wondering why you’re so tired all the time.
glenn mendoza
Thank you for this incredibly thorough and sobering breakdown. As someone who has watched a parent navigate chronic pain and long-term NSAID use, I can attest to how insidious this issue is. The silence of internal bleeding is terrifying-no warning, no pain, just fatigue that gets chalked up to aging. I hope this post reaches the millions who think, ‘It’s just a pill.’ It’s not. It’s a commitment to your body’s long-term health. Please, if you’re on daily NSAIDs, talk to your doctor-not just about pain, but about protection. A PPI isn’t a ‘side effect fix’-it’s a lifeline.
Randy Harkins
Yessss!!! 🙌 This needs to be on every OTC bottle. I’ve been on low-dose aspirin for 8 years for heart health-no symptoms, no issues. Then last year, my hemoglobin dropped to 9.8. No black stools, no vomiting, just… exhaustion. Turns out, silent GI bleed. My doc said, ‘You’re lucky you came in when you did.’ Now I’m on a PPI + acetaminophen for pain. No more NSAIDs. And guess what? My energy is back. I feel like me again. If you’re on daily painkillers and feel ‘off,’ get your iron checked. Seriously. It’s a simple blood test. Don’t wait until you pass out in the grocery store.
Tori Thenazi
Okay, but… what if the whole NSAID scare is a pharmaceutical conspiracy? I mean, think about it: who profits from PPIs? Who profits from endoscopies? Who profits from ‘testing for H. pylori’? The system wants you scared. They want you on lifelong meds. What if your body just needs rest? Or less sugar? Or less stress? Maybe the ‘bleeding’ is just your body detoxing from modern life? I’ve been off NSAIDs for 3 months and I’ve had zero pain… and I’ve never felt more spiritually aligned. Also, I read this article on a forum where a guy said NSAIDs are linked to alien abductions. Coincidence? I think not. 🤔👁️
Angie Datuin
I’ve been on naproxen for 5 years for arthritis. Never had symptoms. Then I got dizzy and pale last month. Turns out, my iron was at 8. I didn’t even know that was possible. Now I’m on celecoxib with omeprazole. It’s not perfect, but I’m alive. This post made me cry. Not because I’m scared, but because I wish I’d known this sooner. If you’re on daily painkillers, please, get a blood test. Even if you feel fine.
Camille Hall
For anyone reading this and thinking, ‘I’m too young for this to matter’-you’re not. I’m 32, take ibuprofen for migraines, and had a silent bleed last year. No warning. Just fatigue. My doctor said, ‘You’re lucky you’re still standing.’ If you’re using NSAIDs regularly, you’re playing Russian roulette with your gut. I’m not saying quit cold turkey-but talk to someone. A pharmacist. A nurse. A doctor. Ask: ‘Is this really necessary?’ There’s always a better way. You deserve to feel good without risking your life.
Monica Warnick
Okay, so I’ve been taking 81mg aspirin daily since 2019 because my cardiologist said ‘it helps.’ But I’ve also been taking Advil every other day for my knee. I didn’t think it mattered. Then I saw this post. Now I’m terrified. What if I’ve already damaged my gut? Should I get an endoscopy? Do I need to tell my doctor I’ve been lying about how often I take Advil? I feel so stupid. And now I’m Googling ‘can you die from silent GI bleeding’ and I’m crying. This isn’t just information. It’s a wake-up call. I’m done. I’m switching to Tylenol. I’m getting tested. I’m not taking chances anymore.
Ashlyn Ellison
My grandma took aspirin every day. Never complained. Died at 82 from internal bleeding. They didn’t find it until autopsy. She didn’t even know she was at risk. Just thought, ‘It’s good for the heart.’
Frank Baumann
Look, I’m not here to sugarcoat this. I’ve been in the ER three times for NSAID-induced bleeds. First time, I thought I had the flu. Second time, I thought I was anemic from my period. Third time, I was in a coma for 36 hours. I was 39. I had no history of ulcers. No family history. Just took ibuprofen daily for my back. The doctors said I was a walking time bomb. Now I’m on a PPI, a walking cane, and therapy. And I still have chronic pain. But I’m alive. And I’m screaming this from the rooftops: If you’re on NSAIDs daily, you’re not ‘managing pain’-you’re gambling with your life. And you don’t get to pick the outcome. I didn’t. And neither will you.
Chelsea Deflyss
so i was just reading this and i think its so important but like i have this friend who takes 2 advil every night for her headaches and shes 27 and shes fine?? like she doesnt even feel bad?? so maybe its just for older people?? also i think people should just stop being so dramatic about pills?? like its not like its crack or something??
Write a comment
Your email address will not be published. Required fields are marked *