
When a doctor prescribes a pill that contains two or more drugs in one tablet-like a blood pressure combo of an ACE inhibitor and a diuretic-what happens when the pharmacist runs out of that exact brand? Can they swap it for another combination pill with similar ingredients? Or worse, can they give you two separate pills instead? The answer isn’t simple. In fact, it’s legally messy, clinically risky, and varies wildly depending on where you live.
What Exactly Is a Combination Drug?
A combination drug isn’t just two pills in one bottle. It’s a single dosage form-tablet, capsule, injection-with at least two active ingredients designed to work together. Think of ATRIPLA, the HIV treatment that packs efavirenz, emtricitabine, and tenofovir into one pill. Or KEYTRUDA + LENVIMA, a cancer combo approved in 2021. These aren’t random mixes. They’re carefully engineered to improve adherence, reduce pill burden, and sometimes even enhance effectiveness. The FDA defines these as combination products when they include drugs, biologics, or devices in one unit. That’s important. If a product has a drug and a delivery device (like an inhaler with two medications), it’s still a combination product under the law. And that complexity is where the problems begin.Why Substitution Laws Are Out of Date
Most state laws in the U.S. were written decades ago for generic substitution: swapping a brand-name drug like Lipitor for its generic version, atorvastatin. That’s straightforward. Same active ingredient. Same dose. Same manufacturer, just cheaper. But combination drugs break that model. If your prescription is for a pill with Drug A and Drug B, and the pharmacy only has a pill with Drug A, Drug B, and Drug C-can they give you that? Legally, in most states, no. Why? Because adding Drug C means you’re getting something not prescribed. That’s not substitution. That’s starting new therapy. Even more confusing: if you’re on a combination pill and the pharmacy gives you two separate generics instead, is that substitution? Some pharmacists think yes. Courts say no. In the 2022 case Smith v. CVS Caremark, the 9th Circuit ruled that substituting a single combination pill with two separate drugs requires explicit prescriber approval. No exceptions.The Legal Gray Zone: What Pharmacists Can and Can’t Do
Pharmacists aren’t trying to break the law. They’re caught in a system that doesn’t match reality. The Alberta College of Pharmacy says it clearly: substituting a beta-blocker for an ACE inhibitor-even if both treat high blood pressure-is therapeutic substitution. And that requires prescribing authority most pharmacists don’t have. Here’s the real-world mess:- Prescribing by adaptation (changing a prescription at refill) is allowed for single drugs in some states, but not for combination products.
- If a patient’s original combo drug is discontinued, and a new combo with different ingredients is available, pharmacists can’t automatically switch it-even if the new one is cheaper and clinically similar.
- Some states allow substitution if the combination contains the exact same active ingredients as the prescribed product. Others require the brand name to match.
- When a patient crosses state lines, the rules change. A swap legal in Texas might be illegal in California.
Therapeutic vs. Generic Substitution: The Critical Difference
Not all substitutions are created equal. - Generic substitution: swapping Brand X for Generic X. Same ingredients. Same dose. Same delivery. Always allowed if state law permits. - Therapeutic substitution: swapping Drug A for Drug B because they’re “similar enough.” Like replacing metoprolol with atenolol for heart disease. This is where things get dangerous with combos. The Therapeutic Substitution Consensus Group (made up of European experts in pharmacology, law, and ethics) warns that switching based on cost alone can hurt patients. For example, replacing a combo pill with two separate generics might mean one drug is taken at the wrong time, or the extended-release mechanism is lost. That’s not just inconvenient-it’s risky. For drugs with a narrow therapeutic index-like warfarin, lithium, or some seizure meds-even tiny differences in absorption can cause toxicity or treatment failure. And many combination drugs fall into this category.Cost Savings vs. Patient Safety: The Real Trade-Off
There’s no denying the economic pressure. Generic drugs make up 90% of prescriptions in the U.S. but only 23% of drug spending. Combination products? They’re growing fast. The global market hit $184.3 billion in 2022, up 12.7% since 2018. Dr. Jane Chen from ICER estimates that expanding substitution for combo drugs could cut medication costs by 15-25% for chronic conditions like diabetes, heart failure, and HIV. That’s billions saved. But here’s the flip side: the American Heart Association warns that inappropriate substitution in cardiovascular combo therapies could lead to adverse events in up to 8% of patients-especially older adults with multiple conditions. One wrong swap, and you could trigger a stroke, kidney failure, or arrhythmia. The NHS in England has successfully cut £280 million annually by standardizing combo substitutions under strict clinical guidelines. Germany, meanwhile, requires a doctor’s signature for every combo switch. The U.S. is stuck somewhere in the middle-no clear rules, no federal guidance, just a patchwork of 50 state laws.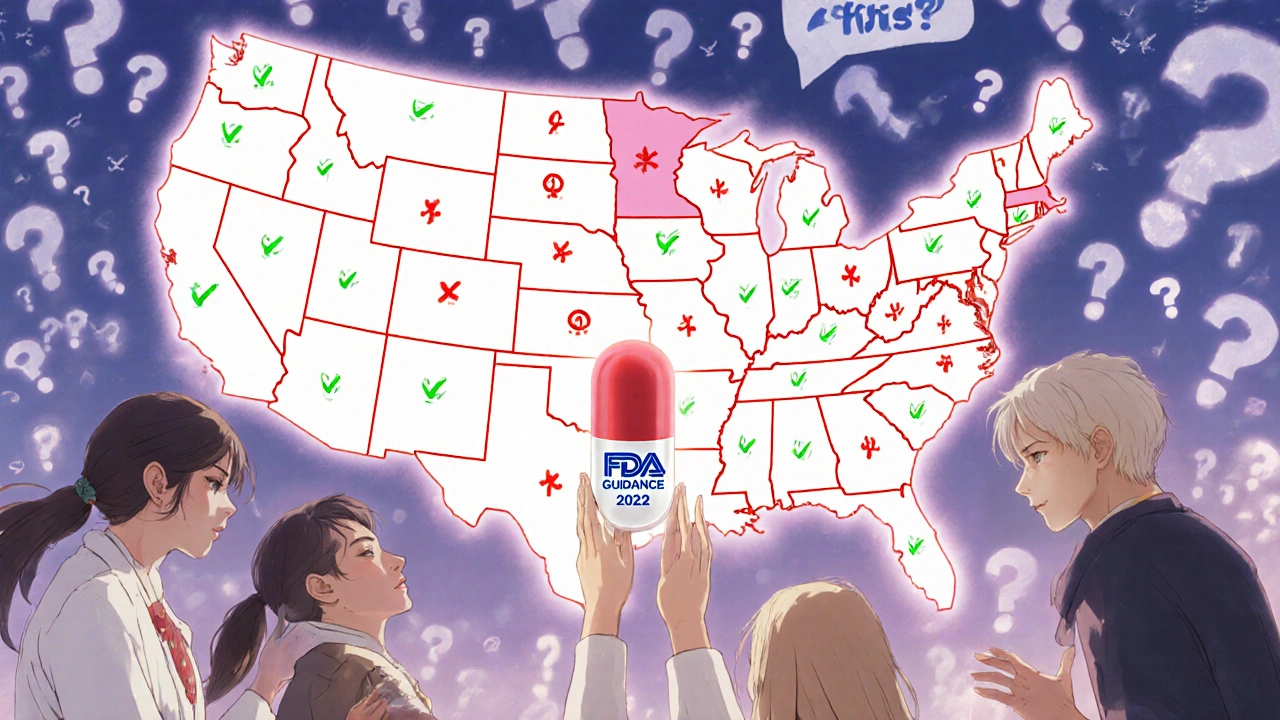
What’s Changing? New Rules on the Horizon
The FDA isn’t ignoring this. In 2022, it released draft guidance on how to prove therapeutic equivalence for fixed-dose combos. That’s a big deal. For the first time, regulators are trying to define what “equivalent” means when you’re dealing with two or more drugs in one pill. The National Association of Boards of Pharmacy proposed a new model law in 2023 that would split combo products into two categories:- Simple combinations: two well-established drugs (like hydrochlorothiazide + lisinopril). These could be eligible for pharmacist substitution under clear criteria.
- Complex combinations: novel drugs, narrow therapeutic index, or new delivery systems (like a combo with a timed-release component). These would require prescriber approval.
What Patients Should Know
If you’re on a combination drug:- Ask your pharmacist: “Is this the exact same combo I was prescribed?” Don’t assume.
- If you get two separate pills instead of one, ask why. Was it a substitution? Was it intentional?
- Check the labels. Are all the active ingredients listed? Are the doses the same?
- If your medication changes without your doctor’s input, speak up. You have the right to know what you’re taking.
What Needs to Happen Next
The system is broken. But fixing it isn’t about banning substitution-it’s about making it smarter. - States need to update laws to distinguish between simple and complex combinations. - Federal guidance is essential. Right now, pharmacists are guessing. The FDA should issue clear standards for therapeutic equivalence in combos. - Electronic prescribing systems must flag combo substitutions. If a pharmacist tries to swap a combo, the system should alert them and require prescriber approval. - Patients need better education. They should understand that a combo pill isn’t just “two pills in one”-it’s a single, calibrated unit. Until then, the burden falls on pharmacists to navigate legal minefields-and on patients to question every change.Can a pharmacist substitute a combination drug without a doctor’s permission?
In most U.S. states, no. If the substitution involves changing the active ingredients-even adding or removing one-the pharmacist is effectively prescribing new therapy. This requires prescriber authorization. Some states allow substitution only if the new product contains the exact same combination of drugs and doses. Others prohibit any substitution of combination products unless explicitly permitted by the prescriber.
Are generic combination drugs easier to substitute than brand-name ones?
Not necessarily. Generic substitution applies when you’re swapping a brand-name combo for its generic version-same active ingredients, same doses. But if the pharmacy doesn’t have that exact generic and offers a different combo with similar but not identical ingredients, that’s therapeutic substitution, not generic substitution. The rules for therapeutic substitution are stricter and vary by state.
Why can’t I just get two separate pills instead of a combo pill?
While it might seem cheaper or simpler, combining two separate drugs doesn’t always replicate a combo pill. Combination products are designed with specific release profiles, ratios, and formulations that can’t be matched by taking pills separately. For example, a combo pill might release one drug slowly while the other acts fast. Separating them could change how they work in your body-potentially reducing effectiveness or increasing side effects.
Do other countries handle combination drug substitution differently?
Yes. The UK’s NHS uses standardized protocols to substitute certain cardiovascular combo drugs, saving millions annually. Germany requires physician approval for nearly all combo substitutions. Denmark allows substitution if the active ingredients match, even if the brand changes. The EU is working on harmonizing these rules, while the U.S. still has 50 different sets of laws.
What should I do if my pharmacist substitutes my combo drug without telling me?
Check the prescription label immediately. Compare the active ingredients and doses to what your doctor prescribed. If they’re different, contact your pharmacist to clarify. If you’re unsure whether the change is legal or safe, call your doctor. You have the right to know exactly what medication you’re taking. Never assume a substitution is safe just because it’s cheaper.






There are 13 Comments
hannah mitchell
Been on a combo pill for hypertension for five years. Never even thought about how it’s legally treated like a bomb until now.
My pharmacist just handed me two separate pills last month. I didn’t ask. Big mistake.
Vanessa Carpenter
I work in a rural pharmacy. We get these questions every week.
Most patients don’t even know the difference between a combo and two pills.
We just try to keep them alive and not get sued.
Bea Rose
So pharmacists are now de facto physicians? Great. Next they’ll be doing MRIs and writing prescriptions for Xanax.
Regulation is a joke when it’s this inconsistent.
Shannon Amos
Let me get this straight.
We pay $200 for one pill that does two things, but if we get two $10 pills instead, it’s ‘illegal’?
Someone’s making money off this mess.
stephen riyo
My dad got switched from his combo pill to two generics last year… he had a mini-stroke three weeks later.
They said it was ‘coincidence.’
My lawyer says it’s not.
And now the pharmacy won’t return my calls.
And I’m not the only one.
And no one’s doing anything about it.
And it’s just… so quiet.
It’s terrifying.
Wendy Edwards
OMG this is so real.
I’ve been on HIV meds for 12 years and ATRIPLA saved my life.
When they switched me to a different combo ‘because it’s cheaper’ I got dizzy for a week and my liver numbers went nuts.
My doc had to fight the insurance for 3 months to get me back on the original.
Don’t let them play Russian roulette with your meds.
And yes, I screamed at the pharmacist.
And I don’t regret it.
Jaspreet Kaur
What is a pill but a promise between chemistry and human need?
When we break that promise for cost, we don’t save money-we break trust.
And trust, once broken, costs more than any drug ever will.
Maybe the real question isn’t what can be substituted-but what must never be touched.
Gina Banh
Simple combo = hydrochlorothiazide + lisinopril. Fine.
Complex combo = a new kinase inhibitor + a timed-release immunomodulator? No.
There’s no reason this can’t be codified.
It’s not hard.
It’s just lazy.
And patients are paying for that laziness.
Deirdre Wilson
I used to think pills were just… pills.
Now I read the labels like a treasure map.
Is this the same magic potion?
Or did they swap the dragon’s breath for a candle?
Douglas Fisher
As someone who’s been on a combo for over a decade-I’ve had this happen three times.
Each time, I had to call my doctor, wait 24 hours, get a new script, and then go back to the pharmacy.
It’s ridiculous.
It’s not just inconvenient-it’s exhausting.
And I’m a healthy, educated, middle-class guy.
What about elderly patients with dementia?
Or people who can’t afford to miss work?
Or those who don’t speak English?
This isn’t a policy issue-it’s a human crisis.
And we’re all just… pretending it’s not happening.
Albert Guasch
It is imperative that regulatory frameworks evolve in tandem with pharmaceutical innovation.
Therapeutic equivalence for fixed-dose combinations must be quantified through bioequivalence studies, not anecdotal clinical experience.
Moreover, the absence of federal standardization constitutes a systemic failure in patient safety governance.
Pharmacists are not physicians, and yet they are being asked to assume prescriptive authority without legal or educational infrastructure.
This is not merely a logistical challenge-it is an ethical imperative for legislative reform.
Without uniform criteria for substitution, we risk creating a two-tiered system of care-one for those who can advocate for themselves, and another for those who cannot.
vikas kumar
India has a similar mess. But we handle it differently.
Pharmacists here can swap if the active ingredients match.
But they’re trained to explain it to patients.
And patients? They ask questions.
Maybe we don’t need more laws.
Just more education.
For everyone.
Michael Collier
Thank you for this comprehensive and necessary exposition.
The current patchwork of state regulations creates unacceptable variability in care delivery.
It is both medically unsound and ethically indefensible to permit substitution protocols to vary based on geography.
Pharmacists are front-line clinicians-they deserve clear, evidence-based guidelines, not legal ambiguity.
Furthermore, the FDA’s draft guidance on therapeutic equivalence for fixed-dose combinations is a critical first step.
It must be finalized without delay and implemented with enforceable standards.
Patients deserve consistency, safety, and transparency-nothing less.
Write a comment
Your email address will not be published. Required fields are marked *