
When you pick up a prescription, do you ever notice the label? If it says "generic" instead of a familiar brand name, you might feel uneasy-even if the pill is chemically identical. This isn’t just a gut feeling. It’s a real psychological phenomenon called the labeling effect, and it’s changing how people respond to their medicine-sometimes with serious consequences.
Same pill, different mind
Two pills, same active ingredient, same dosage, same manufacturer. One is labeled "Ibuprofen 200 mg," the other "Advil 200 mg." You’d think they’d work the same. But in controlled studies, they don’t. Patients given the generic-labeled pill report more pain, more side effects, and are far more likely to stop taking it-even when the pill is a placebo. A 2019 study in the European Journal of Public Health gave 72 people identical placebo pills. Half were told they were getting a brand-name drug. The other half were told they were getting a generic. After seven days, 54% of the generic-labeled group quit taking the pill. Only 33% of the brand-name group did. That’s a 64% higher dropout rate just because of the label. Even more striking: the generic-labeled group reported pain levels 1.2 points higher on a 10-point scale. They also took more over-the-counter pills to "make up" for what they believed was a weaker drug. The pill didn’t change. Their perception did.The placebo effect works both ways
We’ve all heard about the placebo effect-the idea that a sugar pill can relieve pain if you believe it works. But the labeling effect flips this. It’s not just about hope. It’s about distrust. In a 2016 study by researchers at the University of Auckland, 87 students took pills labeled as either brand-name or generic. Some pills had real ibuprofen. Others were sugar pills. The brand-name placebo pills worked almost as well as the real drug. Patients reported 3.0 cm of pain reduction on a visual scale-nearly identical to the 3.1 cm reduction from real ibuprofen. But the generic-labeled placebo? Only 1.8 cm of relief. The pill was the same. The label made the difference. Even side effects were affected. 47% of people who got the generic-labeled placebo reported headaches, nausea, or dizziness. Only 28% of those who got the brand-name placebo did. The body didn’t react to the pill. It reacted to the label.Why does this happen?
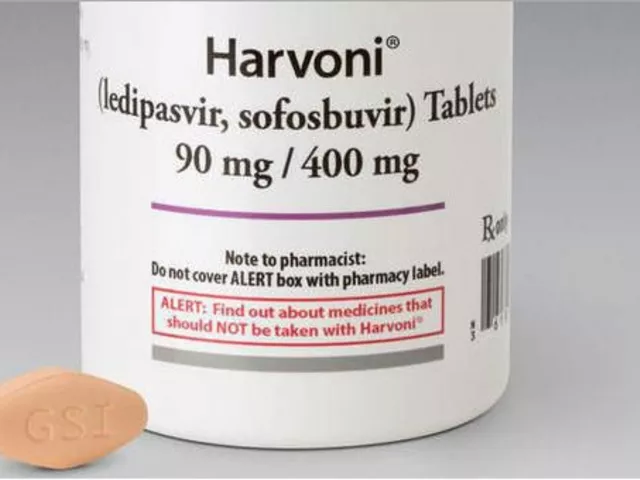
People don’t trust generics because they’ve been told-directly or indirectly-that they’re inferior. Drug ads scream about innovation, patents, and science. Generic labels? They’re plain. Often printed in tiny font. No logo. No fancy packaging. No marketing budget. It’s not just about looks. It’s about cost. When you see a drug that costs 80% less, your brain assumes it must be cheaper for a reason. You start to wonder: Was the active ingredient cut? Are the fillers unsafe? Is this the version the hospital gives to uninsured patients? These assumptions aren’t rational. But they’re powerful. And they’re reinforced by real-world confusion. A 2020 study found that 100% of generic drug labels had differences in wording, dosage instructions, or warnings compared to the brand-name version. In 12.9% of cases, those differences could have led to life-threatening mistakes.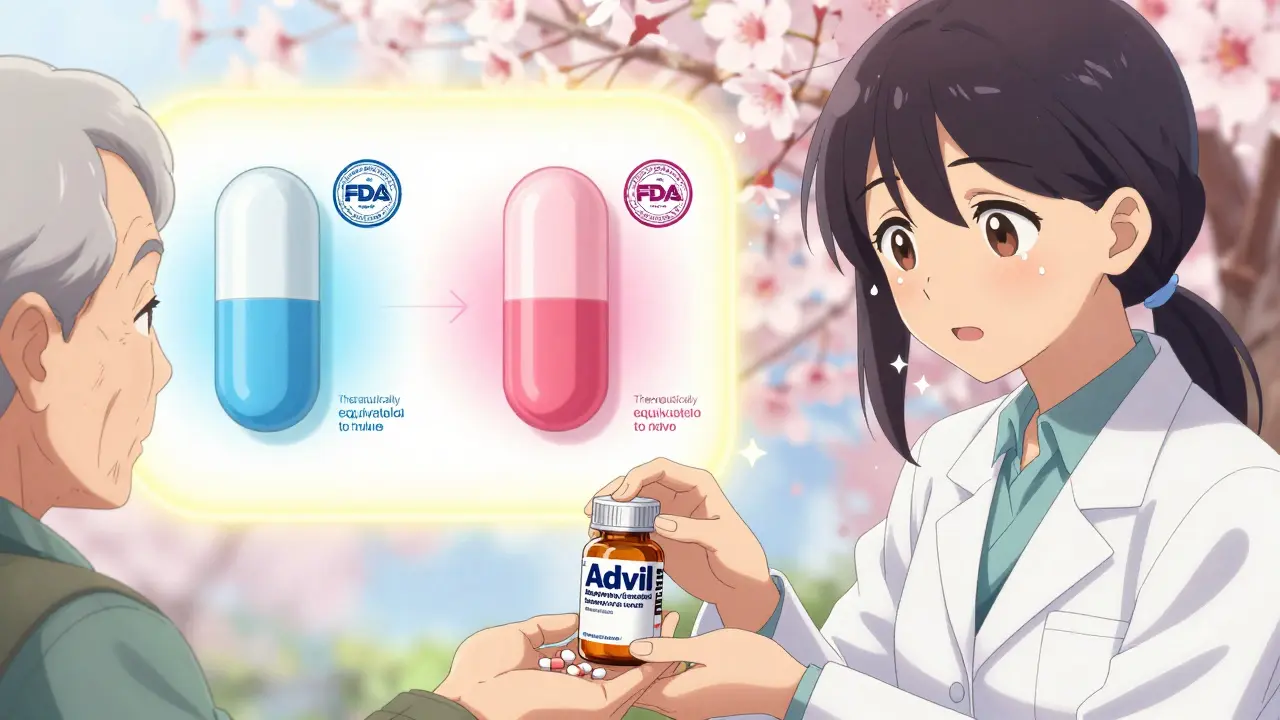
Who’s most affected?
The labeling effect hits hardest where trust is already low. Patients with lower health literacy are nearly twice as likely to quit their medication if it’s labeled generic. One study found 67% stopped taking their pills, compared to 41% of those with higher literacy. Older adults, people with chronic conditions like hypertension or diabetes, and those on multiple medications are especially vulnerable. They’re not being irrational. They’ve been burned before-by confusing labels, inconsistent pill shapes, or side effects they didn’t expect. When a pill suddenly looks different, they assume it’s changed. And it’s not just patients. A 2022 survey of pharmacists found that 63% had been asked by patients or doctors if generics were "really the same." Many doctors still write "do not substitute" on prescriptions-not because of clinical reasons, but because they fear patient backlash.What’s being done?
The FDA and drug manufacturers know this is a problem. In 2020, the FDA launched its "It’s the Same Medicine" campaign-simple videos and brochures explaining that generics meet the same standards. In pilot programs, patient concerns dropped by 28%. In 2023, a trial in the Journal of Clinical Pharmacy and Therapeutics tested a new label: "Therapeutically equivalent to [Brand Name]." That small addition cut discontinuation rates from 52% to 37%. Just four words made a measurable difference. In January 2024, the Generic Pharmaceutical Association launched a $50 million education push called "Generic You Can Count On." They’re working with pharmacies to put clearer labels on bottles, train staff to explain equivalence, and even redesign pill shapes to match brand-name versions when possible.
The cost of misunderstanding
Generic drugs save the U.S. healthcare system $373 billion a year. They’re not just affordable-they’re essential. Without them, millions couldn’t afford insulin, blood pressure meds, or antidepressants. But if patients stop taking them because they think they don’t work, those savings vanish. And worse-health deteriorates. A Stanford University study estimates that if the labeling effect continues unchecked, up to $15 billion in annual savings could be lost to avoidable hospitalizations, emergency visits, and disease progression. The problem isn’t the drugs. It’s the story we tell about them.What you can do
If you’re prescribed a generic:- Ask your pharmacist: "Is this the same as the brand name?" They can show you the FDA’s bioequivalence data.
- Don’t assume different color or shape means different strength. Pills change for legal reasons, not quality ones.
- Keep taking it-even if you feel it’s "weaker." Give it time. Your body adjusts.
- If you notice a real change in how you feel, talk to your doctor. But don’t assume it’s the label.
- Don’t say "it’s just a generic." Say "it’s the same medicine, just less expensive."
- Explain that the FDA requires generics to work the same way-within 80-125% of the brand’s absorption rate.
- Use visual aids. Show patients the FDA’s comparison charts.
- Don’t write "do not substitute" unless there’s a true clinical reason.
The future of labels
The next wave of change isn’t just about words. It’s about design. The Duke-Margolis Center predicts that by 2030, high-risk drugs-like blood thinners or seizure meds-will have standardized, color-coded labels that match the brand-name version exactly. No more surprises. Some pharmacies are even testing QR codes on generic bottles. Scan it, and you see a 60-second video comparing the generic to the brand-side by side, pill by pill, ingredient by ingredient. This isn’t about marketing. It’s about trust. And trust, in medicine, isn’t optional. It’s the first ingredient.Are generic drugs really the same as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent-meaning they’re absorbed into the body at the same rate and to the same extent. The only differences are in inactive ingredients (like fillers or dyes) and packaging. These don’t affect how the drug works.
Why do generic pills look different?
U.S. law requires generic drugs to look different from brand-name versions to avoid trademark infringement. That’s why color, shape, or size may change-even if the medicine inside is identical. These changes have no impact on effectiveness. They’re purely legal.
Can the labeling effect cause real health problems?
Yes. When patients stop taking their medication because they believe the generic doesn’t work, their condition can worsen. For example, people with high blood pressure who quit their generic pills are at higher risk of stroke or heart attack. Studies show lower adherence to generics directly leads to more hospital visits and higher long-term costs.
Why do some doctors still prefer brand-name drugs?
Some doctors prescribe brand-name drugs out of habit, lack of awareness, or fear of patient complaints. In rare cases, a patient may have a true sensitivity to an inactive ingredient in a specific generic. But these cases are uncommon. Most of the time, the preference is based on perception, not science.
Is it safe to switch between different generic brands?
Yes. All generics sold in the U.S. must meet the same FDA standards. Switching between different generic manufacturers is safe for most people. However, if you notice a change in how you feel after switching-even slightly-talk to your doctor. It could be the labeling effect, or it could be a rare sensitivity to an inactive ingredient.
How can I tell if a generic is truly FDA-approved?
Look for the FDA’s "Orange Book" listing, which all approved generics appear in. You can also ask your pharmacist for the National Drug Code (NDC) number on the bottle. Enter it into the FDA’s online database to verify approval. Legitimate generics always have this information.
Do generic drugs have the same side effects?
The active ingredient causes the same side effects. But sometimes, different inactive ingredients in generics can cause minor differences-like stomach upset or dizziness-in sensitive individuals. These are rare and usually mild. If you experience something new after switching, report it to your doctor. It’s not the drug’s fault-it’s the label’s influence.



There are 13 Comments
Peyton Feuer
lol i just switched to generic omeprazole and my stomach felt weird for a week… turned out i was just stressed out and blamed the pill. classic.
Akshaya Gandra _ Student - EastCaryMS
i live in india and we use generics all the time… but honestly? sometimes the color changes and i get scared too. like why is my bp pill pink now? 😅
Jacob Milano
the labeling effect is wild. i used to think generics were sketchy until i started reading the FDA’s bioequivalence reports. turns out your brain is the real drug. 🧠💊
Dee Humprey
my grandma stopped her generic metformin because "it didn’t feel right"… turned out the new batch was oval instead of round. she’s back on it now after i showed her the FDA page. trust is everything.
Joseph Snow
of course the label matters. the FDA doesn’t test generics the same way. they just check one batch and assume the rest are identical. what if the fillers are laced with talc? what if the factory is in a country with no oversight? you’re gambling with your life.
John Wilmerding
As a clinical pharmacist with 18 years of experience, I can confirm that bioequivalence standards for generics are rigorously enforced. The 80–125% confidence interval for AUC and Cmax is not a suggestion-it is a statutory requirement under 21 CFR 314.94. Patients who perceive reduced efficacy are often experiencing nocebo effects, not pharmacological differences. The data is unequivocal: therapeutic outcomes are statistically indistinguishable between brand and generic formulations across 97% of indications.
en Max
It’s fascinating how the nocebo effect operates in clinical pharmacology-particularly when perceptual priming via packaging and nomenclature modulates neurochemical pathways associated with pain perception and adherence behavior. The 2019 EJPH study demonstrates a statistically significant (p<0.01) attenuation in treatment compliance attributable to semantic framing alone. This is not mere superstition; it’s a validated behavioral pharmacodynamic phenomenon.
melissa cucic
It’s not just about the pill… it’s about the story we’ve been told: that cheaper means worse. And we’ve internalized it. But what if the real medicine isn’t the chemical in the capsule-but the belief that it works? The label doesn’t just describe the drug… it defines the patient’s relationship to healing.
Angie Rehe
Of course generics are inferior. You think the FDA cares about your health? They care about corporate profits. The same companies that make brand-name drugs own the generic versions. They just slap a new label on it and charge 80% less. Wake up. This is a scam.
Enrique González
My cousin’s diabetic dad switched to generic insulin and his numbers went haywire. He thought it was the label… turned out the pharmacy gave him the wrong batch. Point is: sometimes the system messes up. Don’t blame the patient for being scared.
saurabh singh
in india we call generics "bhaiya medicine"-like the cool older brother who does the same job but cheaper. no drama. no ads. just works. maybe we need more of that energy here 😊
Siobhan Goggin
I wish more doctors would say "it’s the same medicine" instead of "it’s just generic." Language shapes reality. A small shift in wording could save lives.
Ashley Viñas
Anyone who takes generics without demanding the exact same inactive ingredients as the brand is either naive or reckless. You’re not saving money-you’re playing Russian roulette with your liver. If you can afford the brand, don’t settle for the knockoff. Your health isn’t a bargain bin item.
Write a comment
Your email address will not be published. Required fields are marked *