
Imagine you’re traveling from Australia to Switzerland and your doctor prescribes a common generic blood pressure pill. Back home, it costs $5 a month. In Zurich, the exact same pill-same active ingredient, same dose, same manufacturer-costs $40. Why? The answer isn’t about quality. It’s about policy, profit, and power.
Same Drug, Different Worlds
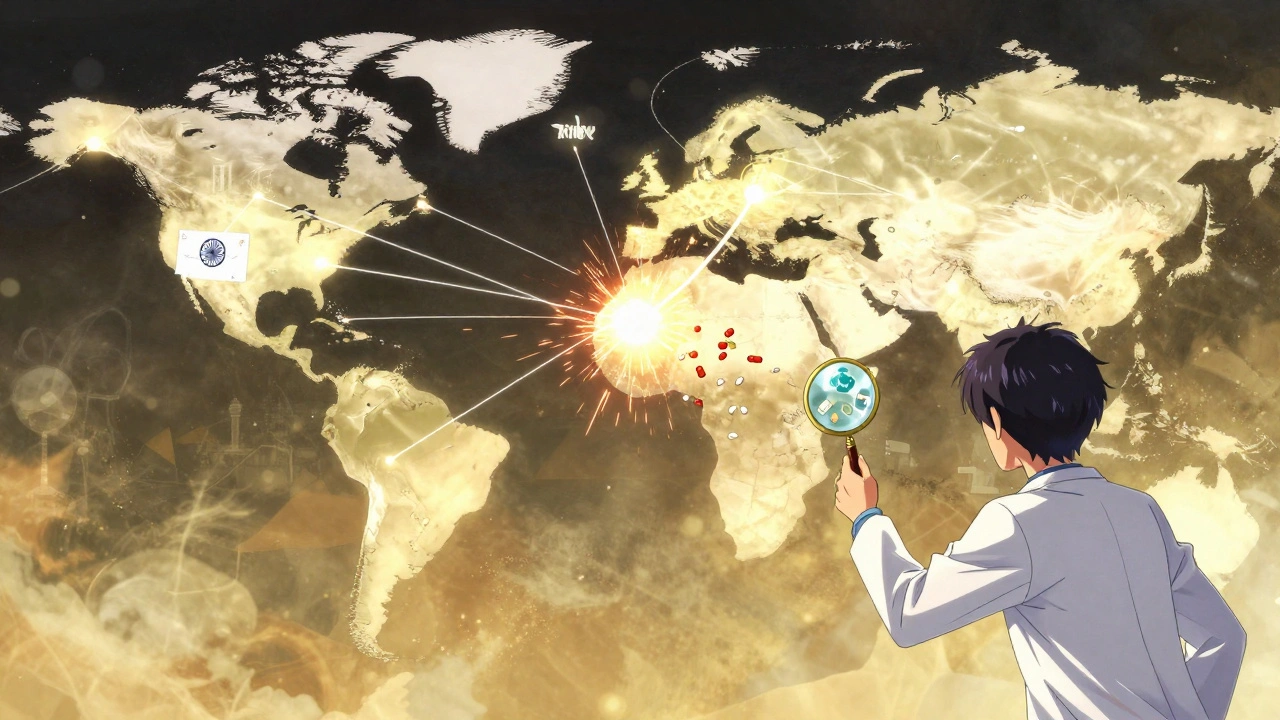
Generic drugs are supposed to be the equal-cost alternative to brand-name pills. They contain the same active ingredients, work the same way, and are held to the same safety standards. But globally, their availability and price vary wildly. In the United Kingdom, 83% of all prescriptions are filled with generics. In Switzerland, it’s just 17%. That’s not a difference in need. It’s a difference in system.The U.S. leads in volume-over 90% of prescriptions are generics. Yet Americans pay more for these same drugs than almost any other country. In 2022, U.S. drug prices (including generics) were 2.78 times higher than in other OECD nations. Meanwhile, India produces 40% of the generic drugs consumed in the U.S., yet pays less than a third of the price for the same medicines. This isn’t a glitch. It’s how the system was built.
Who Decides What’s Available?
It’s not just about patents. Once a brand-name drug’s patent expires, any manufacturer can make a generic version. But whether they actually do-and whether doctors and patients use it-depends on local rules.In the U.S., the FDA requires generics to prove they’re bioequivalent: they must deliver the same amount of active ingredient into the bloodstream within a narrow range (80-125%) of the brand. That’s strict. But in Europe, the European Medicines Agency uses similar standards, yet countries like Germany and the Netherlands push doctors to prescribe generics by law. In Italy and Greece, there’s no such push. Doctors often stick with brands, even when generics are cheaper and approved.
Canada has a unique twist: it tracks how many manufacturers make each generic. In the U.S., 66% of off-patent drugs have two or more makers. In Canada, it’s 43%. Fewer makers mean less competition, and higher prices-even for generics.
Why Is India the Pharmacy of the World?
India makes about 20% of the world’s generic drugs. Over 750 Indian factories are approved by the FDA. That’s more than any other country. And it’s not just about volume. Indian generics are often 60-80% cheaper than U.S. versions. That’s why so many Americans buy them online from Canadian or Indian pharmacies.But here’s the catch: a 2023 study from Ohio State University found that Indian-made generics were linked to 54% more severe side effects-including hospitalizations and deaths-compared to U.S.-made versions of the same drug. The problem isn’t the active ingredient. It’s the fillers, coatings, and manufacturing controls. When the price drops too low, corners get cut. And when a single factory supplies most of a country’s supply, one quality failure can trigger nationwide shortages.

The U.S. Paradox: High Use, High Prices
The U.S. uses more generics than any other country. But it also pays the most. How? Because competition doesn’t always mean lower prices. In fact, in some cases, it means the opposite.Take the drug metformin, used by over 100 million people worldwide for diabetes. In the U.S., it’s sold by dozens of manufacturers. But prices spiked by over 1,000% between 2012 and 2018. Why? Because a few big companies quietly coordinated pricing. When competition is too fragmented, it’s easier to collude. And when the FDA doesn’t inspect factories unannounced, bad actors slip through.
Meanwhile, in the UK, the government negotiates prices directly with manufacturers. There’s no auction. No middlemen. No surprise spikes. The result? A 90% generic market share-and prices that are a fraction of what Americans pay.
Europe’s Patchwork System
Europe looks like a map of contradictions. Germany and the Netherlands have mandatory generic substitution: pharmacists can swap a brand for a cheaper generic unless the doctor says no. In Switzerland, doctors almost never do. Why? Because patients trust brands. And because the government pays more for them.Regulatory delays make things worse. In the EU, even after the European Medicines Agency approves a generic, each country must approve it separately. That adds 18-24 months to market entry. In the U.S., once the FDA says yes, it’s approved nationwide. That’s why generics reach 80% market share in the UK within 12 months-but take 3-5 years in Italy.
Supply Chains and Shortages
During the pandemic, India banned exports of 26 key generic ingredients. Suddenly, hospitals in the U.S., Canada, and across Europe ran out of antibiotics, blood pressure meds, and antifungals. Why? Because so many countries rely on just one or two suppliers.The FDA recorded 147 generic drug shortages in 2023. Nearly 70% came from quality issues at single-source factories-mostly in India and China. One factory failure can ripple across continents. That’s not a supply chain. It’s a single point of collapse.
What’s Changing?
There are signs of progress. The U.S. Inflation Reduction Act of 2022 gives the FDA more money and power to inspect foreign plants. The WHO now has a global benchmarking tool to measure generic quality across countries. The EU wants 80% generic use by 2030.But big problems remain. Drugmakers keep extending patents with tiny tweaks-new coatings, new dosing schedules-that delay generics for years. In the U.S., over 1,200 of these “evergreening” patents were filed between 2015 and 2022 on just 12 top-selling drugs.
And then there’s biosimilars-the next wave of generics for complex biologic drugs like insulin and cancer treatments. They’re cheaper than brands, but harder to make. U.S. uptake is slow because insurers and doctors don’t trust them yet. That’s changing, but slowly.
What This Means for You
If you’re on a generic drug, here’s what you should know:- Same name, same dose, not always same effect. If you switch brands and feel different, tell your doctor. It might be the fillers, not the active ingredient.
- Buying from overseas pharmacies can save money-but not always safety. Stick to verified sites like PharmacyChecker-approved vendors.
- Don’t assume generics are always cheaper. In some countries, brands are reimbursed more than generics. That’s why doctors prescribe them.
- Shortages happen. If your usual generic disappears, ask your pharmacist for alternatives. Not all generics are created equal.
The global generic drug system isn’t broken. It’s designed that way. Profit, regulation, and trust shape what ends up in your pill bottle. And until those systems align, the same medicine will keep costing different amounts in different places.
Why are generic drugs cheaper if they’re the same as brand-name drugs?
Generic drugs are cheaper because they don’t have to pay for the original research, marketing, or patent protection. The brand-name company spent years and billions developing the drug. Once the patent expires, other companies can copy the formula without those upfront costs. They still need to prove it works the same way-but that’s far less expensive than creating a new drug from scratch.
Can I trust generic drugs made in India or China?
Many generic drugs from India and China meet international safety standards. Over 750 Indian factories are FDA-approved, and China has over 180. But quality isn’t uniform. Some facilities cut corners to lower prices, leading to higher rates of side effects and shortages. The FDA inspects foreign plants-but inspections are often scheduled in advance, giving manufacturers time to prepare. Unannounced inspections, common in the U.S., are rare abroad. Stick to generics from trusted suppliers and report any unusual side effects.
Why does the same generic drug cost so much more in the U.S. than in Europe?
In Europe, governments negotiate prices directly with manufacturers and often set price caps. In the U.S., drug pricing is mostly left to the market. Pharmacies, insurers, and middlemen all take a cut. Even with dozens of generic makers, prices can spike if a few companies control the market. There’s no central price setter, so companies charge what they can get away with.
Why do some doctors refuse to prescribe generics?
Some doctors believe brand-name drugs are more reliable, especially for conditions like epilepsy or thyroid disease where small changes in dosage can matter. Others are influenced by patient preference or reimbursement rules. In Switzerland, for example, insurers pay more for brand-name drugs, so doctors have little incentive to switch. In the UK, pharmacists are required to substitute generics unless the doctor says no-so doctors rarely get asked.
What should I do if my generic drug suddenly stops working?
If you notice new side effects, reduced effectiveness, or a change in how you feel after switching generics, talk to your doctor or pharmacist. It could be a different inactive ingredient-like fillers or coatings-that affects how your body absorbs the drug. Keep the old and new pill bottles to compare. Sometimes, switching back to the original brand or a different generic fixes the issue.
Are there any global efforts to fix these differences?
Yes. The WHO is pushing for standardized quality checks across countries. The EU is trying to speed up generic approvals by harmonizing rules. The U.S. FDA is getting more funding to inspect foreign plants and review complex generics faster. But progress is slow. Political and economic interests keep countries from fully aligning their systems. Until then, the differences will remain.
What’s Next?
The future of generics isn’t just about price. It’s about trust, transparency, and control. AI is starting to help design better generic formulations faster. Some companies are experimenting with blockchain to track drug supply chains. But without stronger global standards, these tools won’t fix the root problem: the system rewards profit over predictability.If you rely on generic drugs, stay informed. Know where yours come from. Ask questions. And don’t assume that cheaper means worse-or that more expensive means better. The truth is usually somewhere in between.






There are 11 Comments
Shawna B
I switched my generic metformin last month and felt weird for a week. Turned out the filler was different. My pharmacist said it’s normal but nobody tells you this stuff.
Jerry Ray
Wow so the system is rigged? Newsflash. The real issue isn’t generics it’s that Americans think medicine should be cheap and magic. You want low prices? Move to India. Or stop acting like your pill is a right not a privilege.
Victor T. Johnson
Think about it 🤔 We’ve turned medicine into a casino where the house always wins. The same molecule can cost $5 or $40 not because of science but because of who holds the paperwork. It’s capitalism with a stethoscope. And we’re all just patients in a waiting room waiting for someone to fix a system that was never meant to be fixed.
They patent the cure then sell the key to the door. The active ingredient doesn’t care where it’s made. But the profit margin? That’s where the soul gets sold.
India makes 40% of our generics but gets paid pennies. Meanwhile in the U.S. we pay 10x and still think we’re getting a deal. Why? Because we’ve been trained to believe that higher price = better quality. It’s psychological conditioning wrapped in a pill bottle.
And don’t get me started on evergreening patents. A company adds a coating to a 50-year-old drug and calls it new. Then they get another 20 years of monopoly. That’s not innovation. That’s legal theft.
WHO wants global standards? Good. But who’s gonna enforce them? The same corporations that profit from the chaos? No thanks. We need public ownership of the supply chain not more audits.
Blockchain? AI? Cute. None of that fixes the root. The root is profit motive. The root is that we let corporations write the rules for our health.
When your insulin costs more than your rent you’re not in a healthcare system. You’re in a rent extraction scheme with IV drips.
And yes I know I sound angry. But I’m not angry. I’m just tired of being told to be grateful for crumbs while the table is stacked with gold.
Nicholas Swiontek
Great breakdown! Really appreciate how you highlighted the filler issue - it’s such a hidden factor. I had a similar experience with thyroid meds. One generic made me jittery, another made me exhausted. Switched back and I felt like myself again. Doctors rarely ask about this but pharmacists know. Talk to yours!
Also huge props to Indian manufacturers. They’re feeding the world and still getting blamed. Let’s not forget the FDA approves 750+ of their plants. That’s not luck. That’s skill. The problem isn’t the makers, it’s the pricing games and lack of oversight.
And yeah, the U.S. paradox is real. More generics used, higher prices paid. It’s like buying 1000 cups of coffee and paying $50 each because no one’s negotiating. We need a single buyer like the UK. Simple. Effective.
Keep pushing for transparency. We’re all in this together 💪
Robert Asel
It is an incontrovertible fact that the disparities in generic drug pricing across jurisdictions are not attributable to manufacturing variance per se, but rather to the structural absence of centralized price negotiation mechanisms in the United States healthcare apparatus. The regulatory equivalency standards, while ostensibly harmonized, are rendered functionally inert in the absence of market intervention. Consequently, the phenomenon of price inflation is not anomalous - it is systemic.
Furthermore, the assertion that Indian-manufactured generics exhibit elevated rates of adverse events is not merely a statistical outlier but indicative of a broader regulatory arbitrage wherein cost minimization supersedes pharmacovigilance. The FDA’s scheduled inspections are not merely inadequate - they are institutionally compromised.
One must therefore conclude that the current paradigm is not merely inefficient - it is ethically untenable.
Shannon Wright
Thank you for writing this. It’s so important to understand that the same pill in your hand might have been made in a factory 8,000 miles away - and that’s not bad, it’s brilliant. But we’ve forgotten that medicine isn’t just chemistry. It’s trust. It’s transparency. It’s accountability.
I’ve been on generic blood pressure meds for 12 years. I’ve switched brands three times. Each time I felt different - not because the drug didn’t work, but because the fillers changed. One had corn starch, another had lactose. I’m lactose intolerant. I didn’t know that until I started reading the labels. No one told me to check.
So here’s what I do now: I ask my pharmacist for the manufacturer name. I Google it. I look up FDA inspection reports. I keep a little notebook. I share it with my friends. We’re not powerless. We just need to know how to use our voice.
And to everyone saying ‘just buy from India’ - please don’t. Not unless you use PharmacyChecker. I’ve seen too many people get counterfeit meds. It’s not worth it. There are safe, affordable options in the U.S. too - you just have to know where to look.
Let’s stop blaming the system and start building better habits. We can do this. Together.
vanessa parapar
Oh wow so you didn’t know generics can be dangerous? Congrats, you just discovered capitalism. Also, if you’re buying from India you’re basically gambling with your life. I know a guy who got hospitalized from a bad batch. Don’t be that person.
Ben Wood
...and yet... the FDA... *sigh*... they inspect... but only when they’re told to... and only on schedule... and only after... well... you get it. The whole thing is a farce. We’re living in a dystopia where your blood pressure pill is a lottery ticket. And no one’s talking about it. Why? Because the people who profit? They own the media. The politicians. The entire damn system. And you? You’re just supposed to swallow it. Literally.
Sakthi s
India makes cheap medicine because we know how to make it right - not cheap. We don’t cut corners. We work hard. Many of us have family on these meds. We care. Don’t assume all Indian drugs are bad. Check the factory. Trust the data. Not the fear.
Rachel Nimmons
Did you know the FDA and WHO are both controlled by Big Pharma? This whole article is a distraction. The real reason prices are high is because they’re injecting tracking chips into the pills. To monitor us. And the shortages? They’re planned. To create fear. So we’ll pay more. I’ve seen the documents.
Robert Altmannshofer
Man. I read this whole thing while on my morning walk. Felt like I was reading a detective novel - but the villain is a patent lawyer and the victim is your grandma’s blood pressure pill.
What stuck with me? The part about Germany forcing pharmacists to swap generics. That’s not magic. That’s policy. We could do that here. But we’d have to choose: profit or people.
And honestly? I’m tired of pretending we’re not making that choice every time we fill a prescription.
Also - shoutout to the Indian factories. They’re the unsung heroes. The world runs on their pills. And we treat them like a dirty secret.
Next time you get a generic? Look at the bottle. Ask where it’s from. Say thanks. Then ask why it costs so much.
Write a comment
Your email address will not be published. Required fields are marked *