
When you’re diagnosed with hormone receptor-positive breast cancer, one of the first big decisions you’ll face is which hormone therapy to take. Two main drugs dominate this space: tamoxifen and aromatase inhibitors. Both work to stop estrogen from fueling cancer growth, but they do it in very different ways-and for different women. Choosing between them isn’t just about which one works better. It’s about your age, your menopausal status, your risk of side effects, and what kind of life you want to live while on treatment.
How Hormone Therapy Stops Breast Cancer
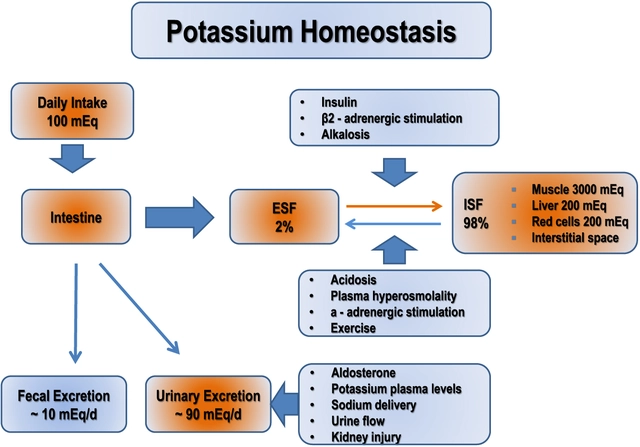
Not all breast cancers are the same. About 8 out of 10 breast cancers are hormone receptor-positive, meaning they grow in response to estrogen. Hormone therapy doesn’t kill cancer cells like chemotherapy does. Instead, it starves them by blocking estrogen’s ability to bind to cancer cells or by cutting off the body’s supply of estrogen altogether. This reduces the chance of cancer coming back after surgery, radiation, or chemo. Tamoxifen has been around since the 1970s. It’s a selective estrogen receptor modulator, or SERM. Think of it like a key that fits into the estrogen lock on breast cancer cells-but instead of turning the lock open, it jams it. That stops estrogen from signaling the cancer to grow. It’s taken as a daily pill, usually 20 mg, and stays active in your body for days after you stop taking it. Aromatase inhibitors (AIs) came later, in the late 1990s and early 2000s. These drugs-like anastrozole (Arimidex), letrozole (Femara), and exemestane (Aromasin)-don’t block estrogen receptors. They shut down the enzyme called aromatase, which turns male hormones into estrogen in fat tissue. In postmenopausal women, the ovaries have stopped making estrogen, so nearly all of it comes from this conversion. AIs reduce estrogen levels by 95% or more. That’s a much deeper cut than tamoxifen, which still lets some estrogen circulate.Who Gets Which Drug?
Your menopausal status is the biggest factor in deciding between tamoxifen and aromatase inhibitors. If you’re premenopausal-meaning you’re still getting your period-tamoxifen is the standard. Aromatase inhibitors don’t work well on their own in women who still have functioning ovaries because the ovaries keep pumping out estrogen. If an AI is needed, it must be combined with ovarian suppression, usually through monthly injections like goserelin (Zoladex). This shuts down the ovaries, mimicking menopause so the AI can do its job. For postmenopausal women, aromatase inhibitors are now the first choice. Large studies like the ATAC trial and the BIG 1-98 trial showed that AIs reduce recurrence risk by about 30% more than tamoxifen over five years. The 10-year breast cancer death rate was lower with AIs too: 12.1% compared to 14.2% with tamoxifen. That’s not just a statistical difference-it means one fewer death for every 30 women treated with an AI instead of tamoxifen. But here’s the catch: AIs aren’t always better for everyone. For younger women with lower-risk cancer, tamoxifen may still be the smarter choice because it protects bone and heart health. In fact, some experts argue that tamoxifen’s long-term benefits in premenopausal women-like lower fracture risk and better cholesterol levels-might outweigh the small edge AIs have in preventing recurrence.Side Effects: What You’ll Actually Feel
No one talks enough about how these drugs make you feel day to day. The side effects aren’t just annoying-they can change your life. Tamoxifen commonly causes hot flashes, night sweats, and mood swings. It also slightly increases the risk of blood clots and, more rarely, endometrial cancer. About 1.2% of women on tamoxifen for 10 years develop endometrial cancer, compared to 0.4% on AIs. That’s why doctors often recommend yearly pelvic exams if you’re on tamoxifen. Aromatase inhibitors? Their biggest issue is joint and muscle pain. Up to half of women on AIs report moderate to severe aches in their hands, knees, or back. Some describe it as arthritis without the swelling. In one survey, 22% of AI users stopped treatment because of this pain, compared to just 8% of tamoxifen users. Bone thinning is another big concern. AIs can cause bone density to drop quickly. About 6.4% of women on AIs suffer a fracture over 10 years, versus 5.1% on tamoxifen. That’s why bone scans (DEXA) are standard for AI users-doctors check your bone health every year or two and may prescribe medications like denosumab if your T-score drops too low. There’s also the brain fog factor. Many women on AIs say they feel more forgetful or mentally sluggish. On online forums, nearly half of AI users mention “chemo brain” getting worse. Tamoxifen users, meanwhile, are more likely to report hot flashes as their main complaint-63% of them, according to one Reddit analysis.
How Long Do You Take It?
The standard is five years. But for women at higher risk of recurrence, doctors now often recommend extending treatment to 7, 8, or even 10 years. The MA.17X and DATA trials showed that going longer reduces the chance of cancer returning, especially in the second half of the decade after diagnosis. Some women start with tamoxifen for 2 or 3 years, then switch to an AI. This “sequential” approach works just as well as starting with an AI right away, according to the OBSERVATION registry. That’s good news if you can’t tolerate an AI from day one. For premenopausal women, if you’re on an AI with ovarian suppression, the standard is still five years. But if you’re on tamoxifen alone, you might stay on it for 10 years if your risk is high.What About Cost and Access?
Tamoxifen is cheap. A generic bottle of 30 pills costs about $15 a month in the U.S., and even less in other countries. Aromatase inhibitors? Brand-name versions can run $150 a month or more. Even with insurance, co-pays can be steep. This gap isn’t just a U.S. problem. In low-income countries, tamoxifen is often the only option because AIs are too expensive or unavailable. That’s why global health experts still call tamoxifen a “life-saving drug” in places where cancer care is limited. In high-income countries, the shift to AIs has been huge. In the U.S., 68% of postmenopausal women now get an AI as first-line treatment-up from 42% in 2010. But even here, cost and access still shape who gets what.
What’s Next? New Drugs on the Horizon
The field isn’t standing still. In 2023, the FDA approved camizestrant, a new oral drug called a selective estrogen receptor degrader (SERD). Unlike tamoxifen or AIs, SERDs don’t just block estrogen-they break down the estrogen receptor itself. In early trials, camizestrant reduced recurrence by 38% compared to standard hormone therapy in women with a specific genetic mutation (ESR1). This could be a game-changer for women whose cancer has become resistant to other hormone drugs. Other studies are testing whether shorter treatment times work. The PERSEPHONE trial is looking at whether three years of tamoxifen is enough for low-risk patients. If it is, that could mean fewer side effects and lower costs for thousands of women. There’s also research into personalized dosing. Some women metabolize tamoxifen poorly because of their genes (CYP2D6 poor metabolizers). These women get less of the active form of the drug and have a higher chance of recurrence. A trial called CYRILLUS is testing whether testing for this gene before starting tamoxifen can help doctors adjust doses or choose a different drug altogether.Choosing the Right Path for You
There’s no single best drug. The right choice depends on your body, your risk, and your tolerance for side effects. If you’re a postmenopausal woman with higher-risk cancer and you can handle joint pain and bone monitoring, an AI is likely your best bet. If you’re younger, have lower-risk cancer, and want to protect your bones and heart, tamoxifen might be the better fit. Talk to your oncologist about your personal risk using tools like the IBIS II calculator. Ask about genomic tests like Oncotype DX-if your score is low, you might not need chemo at all, and hormone therapy alone could be enough. And don’t be afraid to speak up about side effects. If your joints are killing you on an AI, your doctor can help you switch or add bone-protecting meds. If hot flashes are unbearable on tamoxifen, there are non-hormonal options to help. The goal isn’t just to survive cancer. It’s to live well after it. That means choosing a treatment that doesn’t just shrink tumors-but lets you keep living the life you love.Can I take tamoxifen if I’m postmenopausal?
Yes, you can. While aromatase inhibitors are the preferred first choice for postmenopausal women because they reduce recurrence risk more, tamoxifen is still an option-especially if you can’t tolerate AI side effects like joint pain or bone loss. Some women switch from an AI to tamoxifen after a few years if side effects become too difficult. Your doctor will weigh your cancer risk against your quality of life when deciding.
Why can’t premenopausal women take aromatase inhibitors alone?
Aromatase inhibitors only block estrogen made by fat tissue, not by the ovaries. In premenopausal women, the ovaries are still active and produce large amounts of estrogen. If you take an AI without shutting down your ovaries, your body will just make more estrogen to compensate, making the drug ineffective. That’s why premenopausal women need ovarian suppression-usually with injections like goserelin-before starting an AI.
Do aromatase inhibitors cause weight gain?
Weight gain isn’t directly caused by aromatase inhibitors, but many women report gaining weight while on them. This may be linked to reduced estrogen levels slowing metabolism, increased joint pain leading to less activity, or changes in appetite. Tamoxifen has less of an impact on metabolism, which is one reason some women find it easier to maintain weight on tamoxifen.
How do I know if I’m a CYP2D6 poor metabolizer?
You can get tested with a simple saliva or blood test that checks your CYP2D6 gene. This test is not yet routine in all clinics, but it’s becoming more common, especially if tamoxifen isn’t working as expected or if you’ve had a recurrence. If you’re a poor metabolizer, your doctor might switch you to an aromatase inhibitor (if you’re postmenopausal) or consider a higher tamoxifen dose under close monitoring.
Can I stop hormone therapy early if side effects are too bad?
Stopping early increases your risk of cancer coming back. But if side effects are severe, you don’t have to suffer in silence. Talk to your oncologist about alternatives: switching drugs, lowering the dose temporarily, adding medications for joint pain or hot flashes, or taking a short break. Many women find relief by switching from an AI to tamoxifen-or vice versa. The goal is to find a balance between effectiveness and quality of life.



There are 11 Comments
Cara Hritz
so i took tamoxifen for 5 years and honestly the hot flashes were worse than chemo? like i’d wake up drenched at 3am and my husband started sleeping on the couch. also forgot my kid’s birthday because my brain was just… gone. but at least no joint pain. i’m alive, right?
Johnnie R. Bailey
There’s a quiet dignity in choosing survival over comfort. Tamoxifen doesn’t just block estrogen-it forces you to reckon with your body’s betrayal. Aromatase inhibitors? They don’t just steal estrogen-they steal your mobility, your sleep, your sense of self. Both are quiet wars. One waged inside the cell, the other inside the bones. The real question isn’t which drug wins-it’s which version of yourself you’re willing to become to keep living.
Tony Du bled
my aunt did the tamoxifen → AI switch after 3 years. said the joint pain hit like a freight train. now she walks with a cane and takes glucosamine like candy. still alive, still mad at her oncologist. but hey, at least she didn’t get a clot.
Art Van Gelder
Let me tell you something about estrogen-it’s not just a hormone, it’s the invisible architecture of a woman’s body. Tamoxifen jams the door. Aromatase inhibitors burn the whole house down. And then we wonder why women feel like ghosts in their own skin. The real tragedy isn’t the cancer-it’s that we’ve turned survival into a series of trade-offs where your bones, your brain, your libido, your sleep-all become collateral. We call it treatment. I call it slow erasure. And we’re still surprised when women stop taking the pills.
Jamison Kissh
Has anyone looked at the long-term cognitive effects beyond ‘brain fog’? I’m not talking about forgetfulness-I mean actual executive function decline over 10+ years. There’s data on bone density, but almost nothing on neurodegeneration risk. If you’re on AIs for a decade, are you trading breast cancer recurrence for early-onset dementia? I’m not saying yes-but shouldn’t we be asking?
Jim Brown
It is imperative to acknowledge that the medical paradigm has, in many respects, prioritized statistical reductionism over individualized human experience. While AIs demonstrate superior recurrence metrics in population studies, the qualitative burden of arthralgia, osteoporosis, and psychological sequelae cannot be quantified by hazard ratios. A patient’s quality of life is not a secondary endpoint-it is the primary outcome.
Vikrant Sura
lol why are we even talking about this. tamoxifen is a 50 year old drug. ai's are newer so they must be better. also tamoxifen causes cancer? no thanks. case closed.
Candy Cotton
As a U.S. citizen who has read the clinical guidelines, I find it irresponsible that anyone would even consider tamoxifen over an AI for postmenopausal women. The data is clear. If you can’t tolerate side effects, that’s your problem-not the science. We don’t let people choose pain over survival in other cancers. Why here?
Kathryn Weymouth
I was on tamoxifen for 10 years. My bone density stayed normal. My cholesterol improved. I had hot flashes, yes-but I managed them with black cohosh and a fan. I switched to an AI after 7 years because my oncologist pushed it. Within 3 months, I couldn’t open a jar. My knees felt like ground glass. I went back to tamoxifen. I’m 12 years out. No recurrence. My doctor said I ‘defied the guidelines.’ I say I listened to my body.
Nader Bsyouni
so like… what if the whole estrogen thing is just a scam? like maybe cancer just grows because we’re stressed and eat too much sugar? why are we blaming hormones? also tamoxifen is basically just a fancy antidepressant for your boobs
Julie Chavassieux
I switched from AI to tamoxifen after 18 months. My joints screamed. My therapist said I had ‘treatment trauma.’ Now I’m on a low dose. I’m not cured. I’m not a statistic. I’m just… here. And that’s enough.
Write a comment
Your email address will not be published. Required fields are marked *