Bioequivalence: What It Means for Generic Drugs and Your Health
When you hear bioequivalence, the scientific standard that proves a generic drug performs the same way in the body as its brand-name counterpart. Also known as therapeutic equivalence, it's the quiet rule that keeps millions of people on affordable meds without sacrificing results. This isn’t marketing fluff—it’s hard science. If two drugs are bioequivalent, they release the same amount of active ingredient at the same speed. Your body absorbs them the same way. Your blood levels stay steady. Your condition stays controlled. No guesswork. No risk.
But here’s the catch: not every generic drug you see on the shelf has been proven bioequivalent. Some are approved based on paperwork alone, while others go through full clinical testing. The FDA and other global agencies require bioequivalence studies for most generics, but the rules vary by country. In Mexico, where many people rely on lower-cost medications, understanding this concept is critical. A pill labeled "generic lisinopril" might work just like Zestril—or it might not, if the manufacturer skipped proper testing. That’s why you need to know what to look for: active ingredient, dosage, release profile, and whether the maker has a track record. Brands like Teva, Sandoz, and Mylan are often trusted because they’ve repeatedly passed bioequivalence tests. Smaller, unknown labs? That’s where you dig deeper.
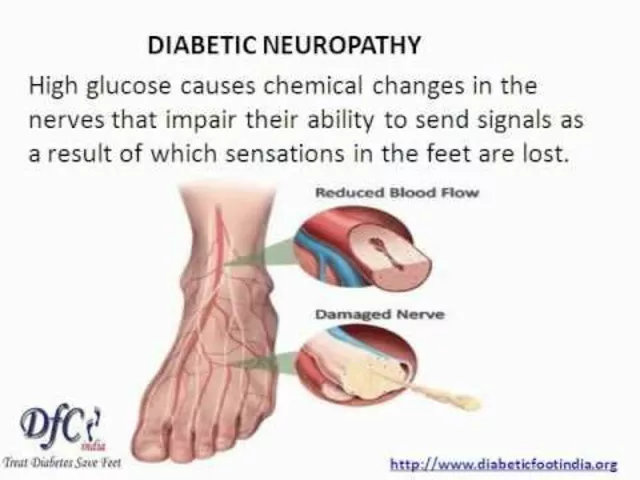
Bioequivalence doesn’t just matter for blood pressure pills. It applies to antidepressants, antibiotics, insulin, birth control, and even supplements like iron or folic acid. If you’ve ever switched from one generic to another and felt different—more tired, more anxious, or worse symptoms—you’re not imagining it. Small differences in fillers or coating can change how fast the drug gets into your system. For drugs with a narrow therapeutic window, like warfarin or thyroid meds, even a 10% variation can be dangerous. That’s why doctors often stick with one brand or generic once it works. Your body gets used to the exact release pattern.
And let’s not forget the link between bioequivalence and generational attitudes. Older adults often distrust generics because they remember when some early versions didn’t work right. Younger people? They’re more likely to trust the price tag and skip the questions. But science doesn’t care about age—it cares about data. Bioequivalence studies are the bridge between fear and confidence. They’re why you can safely switch from brand-name metformin to a generic version and still control your diabetes. They’re why you can buy cheap acetaminophen online without risking liver damage. And they’re why some antibiotics, like tetracycline or cefdinir, might fail if the generic version doesn’t match the original’s absorption rate.
What you’ll find in the posts below are real-world examples of how bioequivalence plays out—sometimes perfectly, sometimes dangerously. You’ll see comparisons between brand and generic versions of lisinopril, atorvastatin, seroquel, and more. You’ll learn how to spot a reliable generic, when to push back on a pharmacy switch, and why your doctor might prefer one version over another. This isn’t about brand loyalty. It’s about making sure your medicine does what it’s supposed to—without costing you extra.