
Every year, millions of people take benzodiazepines for anxiety, insomnia, or seizures. But for many, especially older adults, the cost isn’t just financial-it’s cognitive, physical, and deeply personal. These drugs don’t just calm nerves; they quietly steal memories, unbalance steps, and create dependencies that are hard to break. If you or someone you care about has been on benzodiazepines for months or years, you need to understand what’s really happening inside the brain-and how to get off safely.
How Benzodiazepines Hurt Memory
Benzodiazepines like diazepam, lorazepam, and alprazolam work by boosting GABA, a calming neurotransmitter in the brain. That’s why they help with panic attacks and sleep. But that same mechanism disrupts how new memories are formed. The hippocampus, the brain’s memory center, gets suppressed. You might forget where you put your keys, what you ate for lunch, or even a conversation you had five minutes ago. This isn’t normal forgetfulness-it’s anterograde amnesia, meaning you can’t make new memories while the drug is active. Studies show this effect is strong across all benzodiazepines, though some hit harder than others. High-potency drugs like alprazolam cause sharper memory drops than longer-acting ones like diazepam. But even diazepam, often thought of as "gentler," still impairs recall. One review of 12 studies found that people on benzodiazepines performed 30% worse on memory tests compared to those not taking them. And it’s not just short-term. Long-term users-those on the drugs for over a year-show measurable declines in working memory, processing speed, and visuospatial skills. Some lose up to 15 IQ points over time. Worse, these memory problems don’t vanish when you stop. A 2023 meta-analysis tracked 1,800 former users after they quit. Even six months later, 55% still struggled with recall, attention, and mental clarity. Brain scans showed no permanent damage, but the brain’s ability to process information remained sluggish. It’s like the system is still running in slow mode.Falls Aren’t Just Accidents-They’re a Drug Side Effect
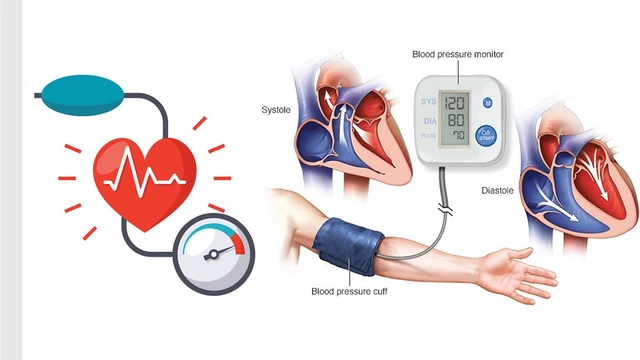
Falls in older adults aren’t always about weak muscles or slippery floors. Often, they’re caused by a pill on the nightstand. Benzodiazepines reduce reaction time by 25-35% and impair balance control by up to 40%. That means when you trip on a rug or reach for something on a high shelf, your body can’t correct itself fast enough. Data from 25 studies involving over a million people found that benzodiazepine users had a 50% higher chance of falling and a 70% higher risk of breaking a hip. In the U.S. alone, these drugs contribute to about 93,000 emergency room visits from falls every year-mostly in people over 65. The risk isn’t just about age. It’s about dose and duration. Someone taking 10 mg of diazepam daily is far more likely to fall than someone on 2 mg. And switching from a long-acting drug like chlordiazepoxide to a short-acting one like lorazepam can spike the risk even more. The American Geriatrics Society has labeled benzodiazepines as "potentially inappropriate" for seniors since 2012. Yet, they’re still prescribed. Why? Because doctors often don’t realize how dangerous they are-or because patients are too anxious to stop. But the numbers don’t lie: if you’re over 65 and on benzodiazepines, your risk of a serious fall is higher than if you had uncontrolled high blood pressure.Tapering Isn’t Optional-It’s Necessary
Stopping benzodiazepines cold turkey can trigger seizures, extreme anxiety, hallucinations, and even psychosis. Withdrawal isn’t just uncomfortable-it’s dangerous. That’s why tapering isn’t a suggestion. It’s a medical requirement. The gold standard is the Ashton Protocol, developed in the 1980s and still used today. It says: switch from your current benzodiazepine to diazepam (because it’s long-acting and metabolizes slowly), then reduce the dose by 5-10% every 1-2 weeks. For someone on 20 mg of diazepam daily, that means dropping 1-2 mg every two weeks. That’s slow. But speed kills here. A 2021 trial with 312 long-term users found that using this method, 68.5% successfully quit after six months. Those who rushed-cutting doses by more than 15% per week-had a 60% failure rate. The key isn’t just the speed-it’s consistency. Many people need to pause the taper for 2-4 weeks if symptoms like brain fog, dizziness, or insomnia return. That’s normal. It’s not a sign you’re failing. It’s your brain adjusting. One of the biggest surprises? Cognitive improvement starts fast. By week 4, people in the trial showed a 15% boost in processing speed. By week 8, attention improved by nearly 20%. Memory didn’t bounce back overnight-but it did come back. And for those who stuck with it, 73% reported better focus and mental clarity within a year.
What Works When Tapering
There’s no magic pill to make tapering easy. But there are proven strategies:- Use diazepam for tapering, even if you were on something else. Its slow breakdown gives your brain time to adapt.
- Reduce by 2-5% per month if you’ve been on benzodiazepines for more than five years. Slower is safer.
- Track your progress with apps like BrainBaseline or a simple journal. Note your mood, sleep, and memory each day. Small improvements matter.
- Don’t do it alone. Work with a doctor who understands tapering. Many general practitioners don’t. Seek out a psychiatrist or addiction specialist if needed.
- Support matters. Online communities like Benzodiazepine Information Coalition and Reddit’s r/benzowithdrawal have over 23,000 members who’ve been through it. Their advice? "Be patient. Your brain is rewiring. It takes time."
When You Shouldn’t Stop
Not everyone needs to quit. Some people-especially those with severe epilepsy or treatment-resistant anxiety-may need long-term use. But even then, the rules are clear:- Use the lowest effective dose. For people over 65, that’s no more than 5 mg of diazepam daily.
- Get cognitive screening every six months. If your MoCA score drops by 3 points or your MMSE drops by 2, it’s time to reconsider.
- Re-evaluate every year. Ask: "Is this still helping? Or is it just keeping me numb?"

The Future: Better Options Are Coming
The good news? New drugs are on the horizon. Researchers are developing GABA-targeting medications that calm anxiety without touching memory. Early trials of α2/α3-selective agonists show 70% reduction in anxiety-with no memory loss. These aren’t available yet, but phase III trials are underway. In the next five years, we may finally have anxiety treatments that don’t cost your brain. Until then, the choice is simple: keep taking a drug that dulls your mind and risks your safety-or begin a slow, careful taper that gives your brain back its clarity.Can benzodiazepines cause permanent brain damage?
No, benzodiazepines don’t cause structural brain damage like a stroke or trauma. Brain scans of long-term users show no shrinkage or lesions. But they do cause functional changes-slowed neural communication, reduced activity in memory centers, and altered receptor sensitivity. These changes can last months or years after stopping, making it feel like permanent damage. The good news? Most cognitive functions improve over time with proper tapering and support.
How long does it take to recover memory after stopping benzodiazepines?
Recovery varies. Some people notice better focus within 4-8 weeks of starting a taper. Memory and attention typically improve steadily over 6-12 months. A 2023 study found that only 45% of long-term users returned to normal cognitive levels after 10 months. For others, full recovery takes up to two years. Patience and consistency are critical. Avoid alcohol, sleep deprivation, and stress during this time-they slow healing.
Is it safe to taper benzodiazepines on my own?
It’s not recommended. Withdrawal can cause seizures, panic attacks, and hallucinations. Even if you feel fine, your body might be under stress. A doctor can help you switch to diazepam, set a safe taper schedule, and monitor for complications. If you can’t access a specialist, reach out to a pharmacist or mental health clinic-they often have resources for tapering support.
Why is diazepam used for tapering instead of other benzodiazepines?
Diazepam has a long half-life-up to 100 hours-meaning it stays in your system longer and leaves slowly. This avoids the sharp peaks and crashes that happen with short-acting drugs like alprazolam or lorazepam. The smoother decline reduces withdrawal symptoms like rebound anxiety and insomnia. Switching to diazepam first makes the taper more manageable and safer.
What should I do if I feel worse during tapering?
It’s common to feel worse before you feel better. If symptoms become unbearable, pause the taper for 2-4 weeks. Don’t increase your dose back to the original level-that can restart dependence. Instead, hold at your current dose until symptoms stabilize, then try reducing again at a slower rate. Keep a journal of symptoms. Share it with your doctor. Many people succeed after one or two pauses.
Next Steps
If you’re on benzodiazepines and worried about memory or falls:- Ask your doctor for a MoCA or MMSE test. Know your baseline.
- Find out what your current dose is in diazepam equivalents (e.g., 1 mg lorazepam = 10 mg diazepam).
- Research the Ashton Protocol. Print it out. Bring it to your next appointment.
- Join a support group. You’re not alone.
- Start tracking your sleep, mood, and memory daily. Small wins add up.




There are 12 Comments
Mussin Machhour
Just quit my 12-year lorazepam habit using the Ashton method. First month was hell-brain fog, insomnia, panic spikes-but by week 6, I remembered my daughter’s birthday without checking my phone. I’m not ‘cured’ but I’m alive again. Stay the course.
Bailey Adkison
They say benzos cause memory loss but never mention the real culprit-pharma profits. Doctors push these because they’re cheap and insurance pays. The FDA knew this in 1985. They buried the data. You think this is medicine? It’s corporate control disguised as care
Carlos Narvaez
Diazepam tapering is the only rational approach. Anything else is amateur hour. The Ashton Protocol isn’t a suggestion-it’s the gold standard. If your doctor doesn’t know it, fire them.
Harbans Singh
I’m from India and we don’t talk about this much. My aunt was on clonazepam for 15 years. When she finally tapered, she cried because she remembered her husband’s voice again. It’s not just about memory-it’s about coming back to yourself.
Justin James
They’re hiding something bigger. Benzodiazepines don’t just cause memory loss-they’re part of a neural dampening program. The same labs that made these drugs also designed the vaccines. They want a docile population. Why do you think they push them for insomnia and anxiety? It’s not treatment-it’s behavioral control. Look at the funding. Look at the patents. Look who owns the FDA.
Rick Kimberly
While the clinical evidence supporting the Ashton Protocol is robust, it is imperative to acknowledge the heterogeneity of patient responses. Individual pharmacogenomic profiles, comorbid psychiatric conditions, and duration of exposure significantly modulate withdrawal trajectories. A one-size-fits-all taper rate may be suboptimal.
Linda B.
So you want us to quit because memory fades? What about the memory of being able to sleep? The memory of not crying in the shower? The memory of not wanting to die? You talk about brain scans like they’re holy scripture. But what about the brain that’s been screaming for 10 years? Who’s gonna fix that?
Christopher King
THIS IS THE NEW WORLD ORDER. They gave us benzos to make us numb so we wouldn’t notice the economy collapsing, the wars, the surveillance, the lies. You think your memory loss is accidental? It’s engineered. The same people who gave you Paxil gave you the vaccine. The same people who told you to take your pills are the ones who shut down the natural medicine clinics. Wake up. The brain is the last frontier of control. And they’re winning. Unless we fight.
Oluwatosin Ayodele
You all talk like this is new. In Nigeria, we’ve seen this for decades. Doctors hand out diazepam like candy. People don’t taper-they overdose. Then they blame the patient. No one checks MoCA scores. No one asks why. You think this is about science? It’s about power. And the rich don’t take these drugs. They take therapy. The poor take pills.
Jason Jasper
I tapered over 18 months. Took longer than I wanted. But I didn’t crash. I still have bad days. But now I can read a book and remember the plot. That’s enough for me.
Zabihullah Saleh
There’s a poem by Rumi that says, ‘The wound is the place where the Light enters you.’ I didn’t know that until I stopped. The withdrawal was the darkest thing I’ve ever done. But in the quiet after, I heard my own thoughts for the first time in 12 years. Not the drug’s voice. Not the anxiety’s scream. Mine. That’s worth every sleepless night.
Lindsay Hensel
To those who say, ‘Just quit’-you have no idea. To those who say, ‘It’s all in your head’-you’ve never felt your own mind betray you. This isn’t weakness. It’s survival. And every single person who tapers with care? They’re heroes.
Write a comment
Your email address will not be published. Required fields are marked *