
When you're taking protease inhibitors for HIV, your life depends on those pills working exactly as they should. Missing a dose, skipping meals, or even taking a common herbal supplement can throw off your entire treatment. One of the most dangerous but often overlooked interactions is between protease inhibitors and St. John’s Wort. This herbal remedy, popular for mild depression, can drop the levels of your HIV medication by more than half-leading to viral rebound, drug resistance, and treatment failure.
What Happens When St. John’s Wort Meets Protease Inhibitors
St. John’s Wort doesn’t just gently interfere with HIV drugs-it actively dismantles them. The key culprit is hyperforin, a compound found in standard St. John’s Wort extracts at concentrations of 2-5%. Hyperforin turns on powerful enzymes in your liver and gut called CYP3A4 and P-glycoprotein. These enzymes are normally there to help your body clear toxins. But when activated by hyperforin, they start aggressively breaking down protease inhibitors before they can do their job. The result? Your blood levels of drugs like lopinavir/ritonavir can crash by up to 57%. In one 2004 study, the area under the curve (AUC)-a measure of total drug exposure-plummeted by 57%, and peak concentration (Cmax) dropped by 81%. That’s not a minor fluctuation. That’s the difference between a drug that keeps your virus suppressed and one that lets it replicate freely.Why This Isn’t Just a Theoretical Risk
This isn’t a lab curiosity. It’s a real, documented cause of treatment failure. In 2021, researchers at the University of North Carolina studied 2,450 HIV patients on protease inhibitors. They found that 8.3% had detectable levels of hyperforin in their blood-meaning they were taking St. John’s Wort. Of those, 3.1% experienced virologic failure: their viral load shot up, and their CD4 counts dropped. Based on CDC data from 2023, that translates to roughly 27,000 cases of therapeutic failure in the U.S. alone each year. The FDA, European Medicines Agency, and Medsafe New Zealand all issued warnings years ago. Lopinavir/ritonavir labels have carried a contraindication since 2003. But patients still take it. Why? Many don’t realize St. John’s Wort is a drug-not just a “natural” supplement. Others think if it’s sold in a health store, it must be safe. Some even stop their HIV meds temporarily to “cleanse” their system, unaware they’re inviting resistance.The Dangerous Myth: “It’s Natural, So It’s Safe”
The idea that herbal means harmless is deadly here. St. John’s Wort is not like chamomile tea. It’s a potent enzyme inducer, on par with prescription drugs like rifampin. And unlike pharmaceuticals, herbal products aren’t held to the same manufacturing standards. A bottle labeled “St. John’s Wort 300 mg” could contain anywhere from 0.5 mg to 15 mg of hyperforin per dose. Most don’t even list it. A 2022 FDA review found that only 37% of St. John’s Wort products on the market accurately disclose hyperforin content. That means if you buy it off the shelf, you’re gambling with your life. One pill might be low-risk. The next batch from the same brand could be lethal.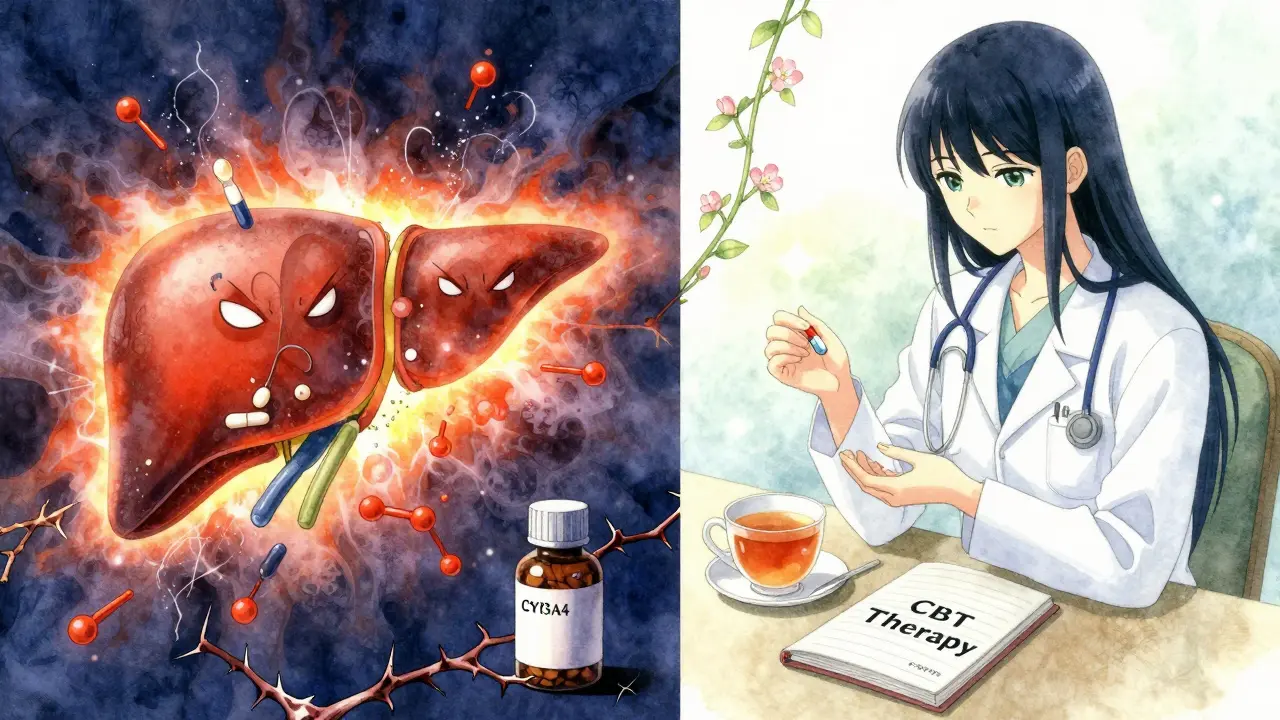
The New Nuance: Low-Hyperforin Formulations
Here’s where things get complicated-and more hopeful. In 2021, researchers discovered that not all St. John’s Wort is equally dangerous. If a product contains 1 mg or less of hyperforin per day, the impact on lopinavir drops to just 12.3%. That’s within the range considered safe for most HIV regimens. The University of Liverpool’s HIV Drug Interactions Database updated its guidance in 2023 to reflect this: coadministration may be considered with low-hyperforin formulations-if the label clearly states the hyperforin content and the daily dose is ≤1 mg. This is a major shift from the old “never mix” rule. But it’s not a green light. It’s a warning to be extremely careful. If you’re considering this route:- Find a product that lists hyperforin content in milligrams per dose-not just “standardized extract.”
- Calculate your total daily hyperforin intake. If it’s over 1 mg, don’t take it.
- Ask your pharmacist to verify the product with the manufacturer’s certificate of analysis.
- Get a viral load test before starting and again after two weeks.
What to Do If You’re Already Taking Both
If you’re currently using St. John’s Wort and taking a protease inhibitor, stop the herb immediately. Don’t wait. Don’t taper. Stop it cold. But here’s the catch: the enzyme-inducing effects don’t vanish when you stop. CYP3A4 stays turned on for at least two weeks. That means your protease inhibitor levels will be low during this time-and then suddenly rise as the enzyme activity fades. This rollercoaster can cause both viral rebound and, later, toxic side effects. Your doctor needs to:- Check your viral load right away.
- Monitor your drug levels if possible.
- Be ready to adjust your protease inhibitor dose after you’ve been off St. John’s Wort for 14 days.

Alternatives to St. John’s Wort for Depression
If you’re using St. John’s Wort because you’re depressed, you’re not alone. Many HIV patients struggle with mood disorders. But there are safer options.- SSRIs like sertraline or escitalopram have no known interaction with protease inhibitors.
- Cognitive behavioral therapy (CBT) is effective for mild to moderate depression and has no drug interactions.
- Exercise, sunlight, and sleep hygiene are proven mood boosters with zero risk.
How to Protect Yourself
Here’s your simple checklist:- Never take St. John’s Wort with any protease inhibitor unless your doctor and pharmacist have approved a verified low-hyperforin product.
- Always tell your HIV provider about every supplement, herb, or OTC drug you take-even if you think it’s harmless.
- Check labels for hyperforin content. If it’s not listed, assume it’s dangerous.
- Use only pharmacies that source products with batch-specific testing.
- Get a viral load test if you’ve ever taken St. John’s Wort, even once.
What’s Next?
Researchers are now working on hyperforin-free St. John’s Wort extracts and point-of-care tests that can detect hyperforin in blood within minutes. These could one day make safe use possible. But for now, the safest choice is simple: avoid it. This interaction isn’t just about one herb and one class of drugs. It’s about the gap between how patients think about “natural” remedies and how medicine actually works. Protease inhibitors are precision tools. St. John’s Wort is a sledgehammer. They don’t belong together.Can I take St. John’s Wort with my HIV meds if I use a low-dose version?
Only if the product clearly states it contains 1 mg or less of hyperforin per day and your doctor confirms it’s safe for your specific regimen. Most store-bought products don’t list hyperforin content, so assume they’re unsafe. Always verify with your pharmacist using the manufacturer’s certificate of analysis.
How long does St. John’s Wort affect my HIV medication after I stop taking it?
The enzyme-inducing effects last at least 14 days after you stop. During this time, your protease inhibitor levels may remain too low to control the virus. After two weeks, levels may rise suddenly, increasing the risk of side effects. Always get a viral load test and work with your doctor before making any changes.
Why do some sources say St. John’s Wort is safe while others say it’s dangerous?
The confusion comes from outdated information. Before 2021, all St. John’s Wort was considered dangerous. Now, research shows low-hyperforin versions (≤1 mg/day) may be acceptable. But since most products don’t disclose hyperforin content, the safest advice remains: avoid it unless you can prove the dose is safe.
Does this interaction happen with all HIV drugs?
No. It primarily affects protease inhibitors like lopinavir, atazanavir, and darunavir. It also interacts with non-nucleoside reverse transcriptase inhibitors (NNRTIs) like efavirenz. But integrase inhibitors (e.g., dolutegravir) and NRTIs (e.g., tenofovir) are not significantly affected. Always check your specific drugs using the University of Liverpool’s HIV Drug Interactions Database.
What should I do if I accidentally took St. John’s Wort with my HIV meds?
Stop taking St. John’s Wort immediately. Contact your HIV provider right away. They’ll likely order a viral load test and possibly a drug level test. Do not restart your HIV meds at your usual dose without medical advice-your body’s metabolism may have changed, and you could be at risk for either treatment failure or toxicity.





There are 11 Comments
Lisa Davies
Just read this and my jaw dropped. I’ve been taking St. John’s Wort for years thinking it was just ‘herbal wellness.’ 😱 My doc never mentioned it. Time to call them tomorrow. Thank you for this wake-up call.
Melissa Taylor
This is exactly why we need better patient education. I work in a clinic and half the people I see don’t even realize supplements can be drugs. The myth that ‘natural = safe’ is killing people. 🙏
Christina Bischof
I used to take it for anxiety. Never knew it could mess with my meds. I stopped cold when I found out. Still feel weird without it but way better than risking my viral load. Just wanted to say thanks for writing this.
Jocelyn Lachapelle
So many people think if it’s in a bottle at the grocery store it’s harmless. I’ve seen friends toss their HIV meds because they ‘wanted to detox.’ This post should be mandatory reading for every HIV clinic waiting room.
Mike Nordby
The data presented here is robust and clinically significant. The 57% reduction in AUC and 81% drop in Cmax are not statistically marginal-they represent a direct threat to virologic suppression. The FDA’s contraindication since 2003 remains valid for the vast majority of commercially available products due to unstandardized hyperforin content. Caution is not merely advisable-it is imperative.
Nupur Vimal
People in India think this stuff is like turmeric tea. My cousin took it with her ARVs and her viral load jumped. She didn’t even know it was a problem. Everyone just buys it off the street. No labels. No warnings. Just ‘good for mood.’ This is why we need to stop pretending herbs are harmless. They’re not. They’re dangerous.
Sai Nguyen
Westerners always think their pills are better than natural remedies. St. John’s Wort has been used for centuries. Now you want to ban it because some companies don’t label properly? That’s corporate control, not science.
John Samuel
Let me be blunt: St. John’s Wort is a pharmacological grenade disguised as a wellness trend. It doesn’t just ‘interact’-it detonates your drug levels. And the fact that people still buy it off Amazon without knowing the hyperforin content? That’s not ignorance. That’s negligence. We need mandatory labeling laws, stat.
Michelle M
It’s strange how we treat plants like they’re innocent, but when a lab synthesizes something identical, it’s a ‘drug.’ The truth is, nature doesn’t care if we call it ‘natural’-it only cares about the chemistry. Hyperforin doesn’t know if it came from a farm or a factory. It just does its job. And that job? It’s killing treatment.
Cassie Henriques
Low-hyperforin formulations are a game-changer. If the product is certified and the dose is ≤1 mg/day, CYP3A4 induction is negligible. This isn’t black-and-white anymore. We need point-of-care hyperforin assays ASAP. Also-has anyone looked into CYP2C9 interactions? Might be a blind spot.
Jake Sinatra
Stop taking it. Immediately. Then call your provider. Don’t wait. Don’t rationalize. Don’t assume ‘it was just once.’ The enzyme induction lingers for two weeks. Your viral load could spike during that window. This isn’t a suggestion. It’s a medical imperative.
Write a comment
Your email address will not be published. Required fields are marked *