
Stimulant Cardiac Risk Assessment Tool
Assess Your Risk
This tool helps you understand your personal risk of heart-related side effects when taking stimulant medications for ADHD. Based on current medical research, it evaluates factors that may increase your risk of cardiac arrhythmias.
Risk Level: Low
You appear to have low risk for cardiac side effects with stimulant medications. Continue monitoring your heart health as recommended by your doctor, but you're likely a good candidate for stimulant therapy with proper medical supervision.
When you or your child starts taking a stimulant for ADHD, the goal is clear: focus better, feel calmer, get through the day without constant overwhelm. But behind that relief, there’s a quiet question many people don’t ask out loud: could this be hurting my heart?
What Stimulants Do to Your Heart
Prescription stimulants like Adderall, Ritalin, and Vyvanse work by boosting dopamine and norepinephrine in the brain. That’s how they improve attention and reduce impulsivity. But those same chemicals also hit your heart. They make your heart beat faster and your blood pressure rise-usually just a little. For most people, that’s harmless. But for some, even small changes can trigger something dangerous: an irregular heartbeat, or cardiac arrhythmia.It’s not just about feeling your heart race. Arrhythmias happen when the electrical signals that control your heartbeat get messed up. Some are harmless. Others can lead to fainting, stroke, or even sudden cardiac arrest. Stimulants interfere with the heart’s natural electrical system by blocking key ion channels-especially potassium and sodium channels. This can lengthen the QT interval on an ECG, a red flag for dangerous rhythms like torsades de pointes. Cocaine and methamphetamine do this dramatically. But even prescription versions can cause similar, though milder, effects.
Who’s at Real Risk?
The risk isn’t the same for everyone. A 2021 study tracking adults over 65 found that within 30 days of starting a stimulant, their chance of developing a ventricular arrhythmia tripled. That’s a big jump. But here’s the catch: after six months, that risk dropped back to normal. It’s not about long-term use-it’s about the first few weeks. Your heart is adjusting.For younger people, the story looks different. A 2024 study showed that long-term stimulant use might slowly lead to heart muscle changes-cardiomyopathy-that could increase arrhythmia risk over years. But again, the absolute risk remains low. Most people won’t develop this. Still, if you have a family history of sudden cardiac death before age 50, or if you’ve had unexplained fainting, chest pain, or a known heart condition, your risk goes up.
Here’s what doctors look for before prescribing stimulants:
- Personal or family history of sudden death, arrhythmias, or heart disease
- Unexplained fainting or dizziness, especially during exercise
- Chest pain or shortness of breath not tied to asthma or anxiety
- Known heart defects, including repaired congenital issues
- Use of other medications that affect heart rhythm
Physical exams check for heart murmurs or irregular pulses. Blood pressure and heart rate are measured before starting, then again at one to three months, and every six to twelve months after that. If numbers climb above the 95th percentile, doctors pause the medication. No ECG is required for everyone-but if any red flags show up, one becomes essential.
The Big Contradiction: Do They Really Increase Risk?
You’ll hear conflicting things. One study says stimulants triple arrhythmia risk in older adults. Another large meta-analysis published in JAMA Network Open in 2022 found no significant link between ADHD meds and heart disease across any age group. Why the difference?It comes down to who’s being studied and how long. Older adults have less heart reserve. Their systems are more fragile. A small spike in adrenaline can push them over the edge. Young people? Their hearts bounce back. Also, many studies compare stimulant users to non-users without accounting for ADHD itself. ADHD is linked to higher rates of smoking, substance use, and poor sleep-all of which hurt the heart. So is it the drug? Or the condition?
The truth? For most people, the benefits outweigh the risks. The American Heart Association and American Academy of Pediatrics agree: routine ECGs aren’t needed for everyone. But they also say: don’t ignore warning signs. If your heart starts skipping, racing, or hurting after starting a stimulant, tell your doctor. Don’t wait.

What Happens If You Have a Heart Problem?
If you have a known arrhythmia, long QT syndrome, hypertrophic cardiomyopathy, or a history of heart failure, stimulants are usually avoided. But not always. Some patients with stable, repaired congenital heart disease can still take them-with close monitoring. Cardiologists and psychiatrists often work together in these cases.Here’s what doctors do when they’re worried:
- Start with the lowest possible dose
- Check heart rate and BP weekly at first
- Do an ECG before and after starting
- Watch for QT prolongation beyond 460 milliseconds
- Have a plan to stop immediately if symptoms appear
Some patients do well on stimulants even with mild heart conditions. Others don’t. That’s why personalized care matters. One size doesn’t fit all.
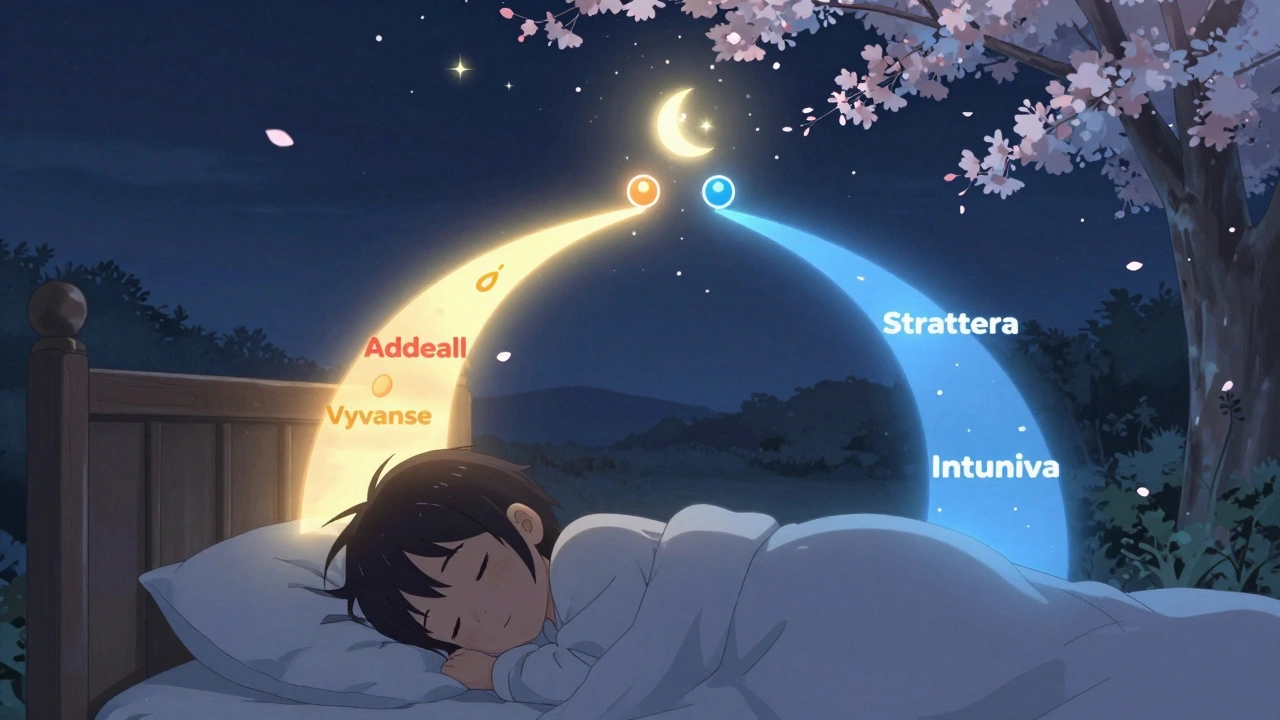
Alternatives That Don’t Stress the Heart
If stimulants feel too risky-or if they’ve already caused problems-there are non-stimulant options. They’re not as fast-acting. They don’t work for everyone. But they’re much gentler on the heart.Atomoxetine (Strattera) is the most common. It’s a selective norepinephrine reuptake inhibitor. It doesn’t cause spikes in heart rate or blood pressure. Studies show it helps about 50-60% of people with ADHD-slightly less than stimulants, but still meaningful. Side effects? Nausea, fatigue, and sometimes mood changes. But no known arrhythmia risk.
Guanfacine (Intuniv) and Clonidine (Kapvay) were originally blood pressure meds. They calm the nervous system by targeting alpha-2 receptors in the brain. They’re especially helpful for kids with impulsivity, emotional outbursts, or sleep issues. They can lower heart rate slightly, which is fine for most. Rarely, they cause dizziness or low blood pressure, so start low and go slow.
Here’s how they compare:
| Medication | Type | Heart Rate Impact | BP Impact | Effectiveness | Time to Work |
|---|---|---|---|---|---|
| Adderall, Vyvanse | Stimulant | Increases (1-5 bpm) | Increases (1-4 mmHg systolic) | 70-80% | 30-60 minutes |
| Ritalin, Concerta | Stimulant | Increases (1-4 bpm) | Increases (1-3 mmHg systolic) | 70-80% | 20-45 minutes |
| Strattera (atomoxetine) | Non-stimulant | Neutral or slight decrease | Neutral | 50-60% | 2-4 weeks |
| Intuniv (guanfacine) | Non-stimulant | Slight decrease | Decreases | 50-60% | 1-2 weeks |
| Kapvay (clonidine) | Non-stimulant | Slight decrease | Decreases | 50-60% | 1-2 weeks |
Non-stimulants take longer to work. You won’t feel a difference overnight. But if your heart is sensitive, that’s a trade-off worth making. Many patients use them alone. Others combine them with low-dose stimulants to reduce side effects.
What to Do Next
If you’re on a stimulant and feel fine-no palpitations, no dizziness, no chest tightness-you’re likely okay. But don’t get complacent. Keep your follow-up appointments. Track your heart rate and blood pressure at home if you can. Use a simple wearable or a manual cuff. Write down any unusual symptoms.If you’re considering starting one, ask your doctor:
- Do I have any red flags in my family or personal history?
- Should I get an ECG before starting?
- What symptoms should I watch for?
- What are the non-stimulant options if this doesn’t work?
If you’re a parent of a child on stimulants, watch for changes in behavior or complaints about their heart. Kids rarely say, “My heart feels weird.” But they might say, “I feel funny,” or “I don’t want to run anymore.” Listen. Then call the doctor.
Final Thought: It’s About Balance
Stimulants change lives. They help people go from failing in school to graduating. From losing jobs to holding them. From constant chaos to calm focus. That’s powerful. But your heart matters too. You don’t have to choose between mental clarity and physical safety. You can have both-by being informed, asking questions, and working with your doctor to find the right fit.The goal isn’t to avoid stimulants. It’s to use them wisely. With awareness. With monitoring. With alternatives ready if needed.
Do stimulants cause heart attacks?
Stimulants rarely cause heart attacks. The risk is extremely low in healthy people. Most cases linked to stimulants involve illicit drugs like cocaine or methamphetamine, or people with undiagnosed heart conditions. Prescription stimulants may slightly increase the chance of arrhythmias in vulnerable individuals, but heart attacks are not a common outcome.
Is it safe to take ADHD meds if I have high blood pressure?
It depends. If your blood pressure is controlled with medication and you have no other heart issues, stimulants may still be an option-but with close monitoring. Your doctor will likely start with a low dose and check your BP weekly at first. If your numbers rise above the 95th percentile, they’ll likely switch you to a non-stimulant like Strattera or Intuniv.
Can I switch from Adderall to Strattera safely?
Yes, but it’s not instant. Strattera takes 2-4 weeks to build up in your system. Your doctor will usually overlap the two medications for a week or two, then slowly taper off the stimulant. This avoids withdrawal symptoms and gives Strattera time to work. Many people find Strattera less effective for focus, but it’s much gentler on the heart.
Should I get an ECG before starting ADHD medication?
Routine ECGs aren’t required for everyone. Major guidelines say they’re only needed if you have symptoms like fainting, chest pain, or a family history of sudden cardiac death. If you’re young and healthy with no red flags, an ECG isn’t necessary. But if your doctor recommends one, it’s a smart precaution.
Are natural alternatives like L-theanine or omega-3s effective for ADHD?
Some people report feeling calmer with omega-3 supplements or L-theanine, but there’s no strong evidence they work as well as FDA-approved medications for core ADHD symptoms like inattention and impulsivity. They may help with anxiety or sleep, which can make ADHD feel better, but they’re not replacements for stimulants or non-stimulants if you need real symptom control.
What to Watch For
If you’re on a stimulant, pay attention to these signs:- Heart palpitations that last more than a few seconds
- Chest pain or pressure, especially during activity
- Dizziness or fainting
- Shortness of breath that doesn’t match your effort
- Unexplained fatigue or weakness
If any of these show up, stop the medication and call your doctor. Don’t wait. It’s better to be safe than sorry.




There are 14 Comments
Rudy Van den Boogaert
My doc never even checked my BP before prescribing. Kinda scary when you think about it.
Ashley Elliott
Chad Handy
Augusta Barlow
Joe Lam
Jenny Rogers
Rachel Bonaparte
Scott van Haastrecht
Chase Brittingham
Bill Wolfe
Ollie Newland
Rebecca Braatz
Michael Feldstein
jagdish kumar
Write a comment
Your email address will not be published. Required fields are marked *